Disorders Of Kidneys.
Category : 11th Class
(1) Pyelonephritis : It is an inflammation of renal pelvis, calyces and interstitial tissue (G.pyelos = trough, tub; nephros = kidney; it is = inflammation). It is due to local bacterial infection. Bacteria reach here via urethra and ureter. Inflammation affects the countercurrent mechanism, and the victim fails to concentrate urine. Symptoms of the disease include pain in the back, and frequent and painful urination.
(2) Glomerulonephritis : It is the inflammation of glomeruli. It is caused by injury to the kidney, bacterial toxins, drug reaction, etc. Proteins and R.B.Cs pass into the filtrate.
(3) Cystitis : It is the inflammation of urinary bladder (G.kystis = bladder, - it is = inflammation). It is caused by bacterial infection. Patient has frequent, painful urination, often with burning sensation.
(4) Uremia : Uremia is the presence of an excessive amount of urea in the blood. It results from the decreased excretion of urea in the kidney tubules due to bacterial infection (nephritis) or some mechanical obstruction. urea poisons the cells at high concentration.
(5) Kidney stone (Renal calculus) : It is formed by precipitation of uric acid or oxalate. It blocks the kidney tubule. It causes severe pain (renal colic) in the back, spreading down to thighs. The stone may pass into the ureter or urinary bladder and may grow, and cause severe pain of blackade. When in bladder, the patient experiences frequent and painful urination and may pass blood in the urine. Surgery may be needed to remove stone and relieve pain.
(6) Kidney (Renal) failure (RF) : Partial or total inability of kidneys to carry on excretory and salt-water regulatory functions is called renal or kidney failure. Result kidney failure leads to (i) uremia, i.e., an excess of urea and other nitrogenous wastes in the blood (G.ouron = urine, haima-blood); (ii) Salt-water imbalance; and (iii) stoppage of erythropoietin secretion.
Causes : Many factors can cause kidney failure. Among these are tubular injury, infection, bacterial toxins, glomerulonephritis (inflammation of glomeruli) arterial or venous obstruction, fluid and electrolyte depletion, intrarenal precipitation of calcium and urates, drug reaction, heammorrhage, etc.
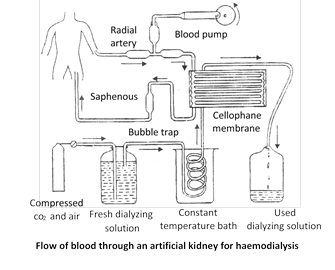
Artificial kidney
Artificial kidney, called haemodialyser, is a machine that is used to filter the blood of a person whose kidneys are damaged. The process is called haemodialysis. It may be defined as the separation of small molecules (crytalloids) from large molecules (colloids) in a solution by interposing a semipermeable membrane between the solution and water (dialyzing solution). It works on the principle of dialysis, i.e. diffusion of small solute molecules through a semipermeable membrane (G. dia = = through, lyo = separate). Haemodialyser is a cellophane tube suspended in a salt-water solution of the same composition as the normal blood plasma, except that no urea is present. Blood of the patient is pumped from one of the arteries into the cellophane tube after cooling it to 0oC and mixing with an anticoagulant (heparin). Pores of the cellophane tube allow urea, uric acid, creatinine, excess salts and excess H+ ions to diffuse from the blood into the surrounding solution. the blood, thus purified, is warmed to body temperature, checked to ensure that it is isotonic to the patient's blood, and mixed with an antiheparin to restore its normal clotting power. It is then pumped into a vein of the patient. Plasma proteins remain in the blood and the pores of cellophane are too small to permit the passage of their large molecules. The use of artificial kidney involves a good deal of discomfort and a risk of the formation of blood clots. It may cause fever, anaphylaxis, cardiovascular problems and haemorrhage. Kidney transplant is an alternative treatment.
Kidney (Renal) Transplantation
Meaning : Grafting a kidney from a compatible donor to restore kidney functions in a recipient suffering from kidney failure is called renal transplantation.
History : First kidney transplant was performed between identical twins in 1954 by Dr. Charles Hufnagel, a Washington surgeon, India's first kidney transplant was done on December 1, 1971 at Christian Medical College, Vellore, Tamilnadu. The recipient was a 35 years old person Shaninughan.
Eligibility : All patients with terminal renal failure are considered eligible for kidney transplantation, except those at risk from another life-threating disease.
Donors : A living donor can be used in a kidney transplant. It may be in identical twin, a sibling, or a close relative. If the living donors are not available, a cadaveric donor may be used (cadaver is a dead body). Over half of the kidney transplants are from cadavers.
Success rate : A kidney transplant from an identical twin, called isogeneic graft or isograft, is always successful. A renal transplant from a sibling or a close relative or a cadaver, termed allogeneic graft or homograft, is usually successful with the use of an immunosupressant that prevents graft rejection by body's immune response. Many renal transplant recipients are known to have retained functional grafts for over 20 years. Earlier, renal transplantation was limited to patients under 55 years. Now, however, with better techniques, kidney grafting has been done in selected patients in the 7th decade of life.
Pretransplant preparation : It includes haemodialysis to ensure a relatively normal metabolic state, and provision of functional, infection-free lower urinary tract.
Donor selection and kidney preservation : A kidney donor should be free of hypertension, diabetes, and malignancy. A living donor is also carefully evaluated for emotional stability, normal bilateral renal function, freedom from other systematic disease, and histocompatibility. Cadaveric kidney is obtained from previously healthy person who sustained brain death but maintained stable cardiovascular and renal function. Following brain death, kidneys are removed as early as possible, flushed with special cooling solutions, such as mannitol and stored in iced solution. Preserved kidneys usually function well if transplanted within 48 hours.
Recipient-Donor Matching : Recipient and donor are tested for 3 factors :
(1) Blood groups : Recipient's blood group should be compatible with donor's blood group.
(2) Human leucocyte antigen (HLA) : It is a genetic marker located on the surface of leucocytes. A person inherits a set of 3 antigens from the mother and three from the father. A higher number of matching antigens increases the chances that the kidney graft will last for a long time.
(3) Antibodies : Small samples of recipient's and donor's blood are mixed in a tube. If no reaction occurs, the patient will be able to accept the kidney.
Transplant procedure : Transplantation is done under general anaesthesia. Operation takes 3 or 4 hours. Cut is given in the lower abdomen. Donor's kidney is transplanted retroperitonealy in the iliac fossa. Artery and vein of new kidney are connected to the iliac artery and vein of the recipient. Ureter of the new kidney is connected to the urinary bladder of the recipient. Often the new kidney starts producing urine as soon as blood flows through it, but sometimes it may take a few weeks before it starts working. A week's stay in the hospital is necessary to recover from surgery, and longer if there are complications.
The new kidney takes over the work of two failed kidneys. Unless they are causing infection or high blood pressure, the old kidneys are left in place.
Immunosupression : Immunosupression means to depress the immune response of the recipient to graft rejection. Prophylactic immunosuppressive therapy is started just before or at the time of renal transplantation. An ideal immunosuppressant suppress immunity against foreign tissue but maintains immunity against infection and cancer. The drug, named cyclosporin, in such an immunosupressant. Use of antiserum to human lymphocytes is equally useful. It destroys T-cell mediated immune responses, but spares humoral antibody responses.
You need to login to perform this action.
You will be redirected in
3 sec
