Process of Respiration
Category : 11th Class
The process of respiration is completed in 4 steps –
(1) Breathing or ventilation
(2) Exchange of gases or External respiration
(3) Transport of gases
(4) Cellular respiration
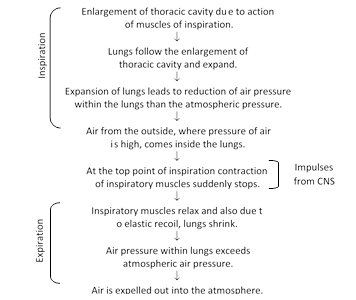
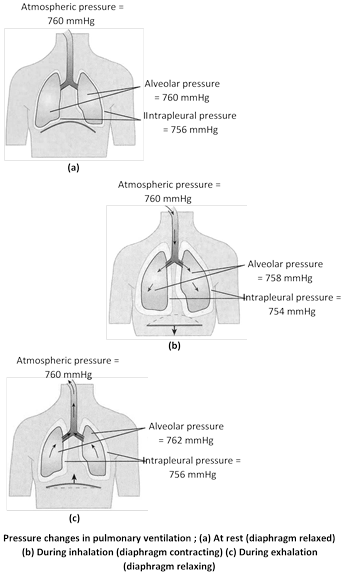
(1) Breathing or ventilation : Movement of thorax, expansion (inflation) and deflation of lungs and flow of air into the lungs and from the lungs. It is extracellular, energy consuming and physical process. Sum of inspiration and expiration is called respiratory movement. There are two steps of breathing -
(i) Inspiration : Intake of fresh air in lungs from outside. It is an active process. Blood pressure increases during later part of respiration. Following muscles are involve in inspiration.
(a) Diaphragm : Principle muscles of inspiration. Its skeletal muscles attached to sternum, vertebral column and ribs. It is formed by radial muscles fibres.
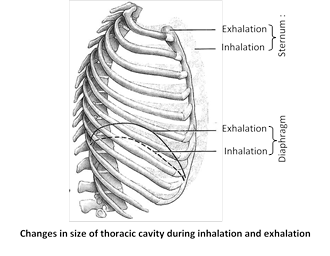
In relaxed condition it is dome shaped. Convex towards thoracic cavity and concave towards abdominal cavity. During inspiration it contract and become straight and descends down. This cause an increase in vertical diameter of thoracic cavity. Descent of diaphragm can explain about 75% of tidal air volume. 70% muscles fibres of diaphragm have some resistance to fatigue. Nerve which supply to diaphragm is phrenic nerve. Contribution of diaphragm in breathing of full term pregnant lady is 0%. Most important function of diaphragm of mammals is to aid in inspiration. If diaphragm is punctured, respiration will stop and patient will die.
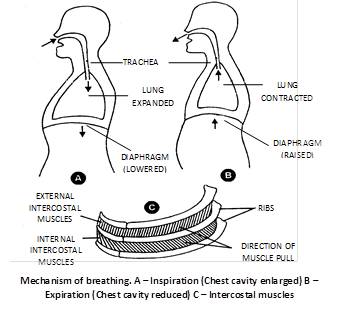
(b) External intercostal muscles : Gaps between the ribs are called intercostal spaces. They are filled by intercostal muscles. Intercostal muscles are of two types external intercostal muscles and internal intercostal muscles.
External intercostal muscles are related to inspiration and internal intercostal muscles are related to expiration. Here we are concerned with external intercostal muscles. External intercostal muscles start from lower border of upper rib and comes to end outer lip of upper border of lower rib. Thus direction of external intercostal muscles fibres is downward forward. Contraction of external intercostal muscles causes increase in anteroposterior diameter of thoracic cavity and transverse diameter of thoracic cavity.
This two dimensional increase in diameter (i.e. anteroposterior and transverse) of thoracic cavity is due to special arrangement of ribs. This increase of thoracic cavity assist by diaphragm the most important muscle of inspiration, it is dome-shaped skeletal muscle. Contraction of diaphragm causes it to flatten lowering its dome. For simplification we can assume that each rib attach anteriorly to sternum by its anterior end and posteriorly to vertebral column by its posterior end. Note these two points carefully -
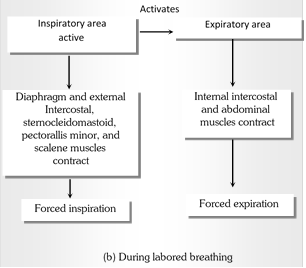
(c) Accessory muscles of inspiration : These muscles normally are not called into action but in forced inspiration they come into action. Accessory muscles are scaleni, sternomastoid and alae nasi.
(ii) Expiration : Out flow of the air from the lungs is called expiration. When the inspiratory muscles relax. As the external intercostal relax, ribs move inferiorly and as the diaphragm relaxes, its dome moves superiorly owing to its elasticity. These movements decrese vertical and anterior-posterior dimentions of thoracic cavity.
(a) Internal intercostal muscles : Direction of fibres is backward and downward. Action is just opposite to external intercostal muscles. These muscles by their action reduce antero-posterior and transverse diameter of thoracic cavity.
(b) Abdominal muscles : Muscles of anterior abdominal wall. These muscles push the diaphragm up.
(iii) Mechanism of ventilation/breathing
(2) Exchange of gases
(i) Exchange of gases in lungs : It is also called external respiration. In this gaseous exchange oxygen passes from alveoli to pulmonary capillary blood and \[C{{O}_{2}}.\] Comes to alveoli from pulmonary capillary. In order to be exchange the gases have to pass through alveolocapillary membrane or respiratory membrane. Composition of alveolocapillary membrane is epithelium lining of alveolar wall, epithelial basement membrane, a thin interstitial space, capillary basement membrane and capillary endothelial membrane.
Thickness of respiratory membrane is \[0.5\,\,\mu \,m.\] Respiratory membrane has a limit of gaseous exchange between alveoli and pulmonary blood. It is called diffusion capacity. Diffusion capacity is defined as volume of gas that diffuse through membrane per minute for a pressure difference of 1 mm Hg. Exchange of gases through alveolocapillary membrane is a purely physical diffusion phenomenon. No chemical reaction is involved. Diffusion of a gas depends upon pressure gradient across the membrane and solubility of gas.
Partial pressure : Partial pressure of a gas is the pressure it exerts in a mixture of gases, and is equal to the total pressure of the mixture divided by percentage of that gas in the mixture. For instance, if the pressure of atmospheric air at sea level is 760 mm. Of mercury (Hg) and oxygen forms 21% of the air, the partial pressure of oxygen will be 21% of 760, or 159 mm. Hg. In other words, the partial pressure of a gas is proportional to its concentration in the mixture. Only about 0.3 ml. of \[{{O}_{2}}\] can dissolve in 100 ml. of plasma, about 20 ml. of \[{{O}_{2}}\] is carried by haemoglobin in 100 ml. of blood. In atmospheric air except these gases some traces of helium, argon and neon are also found.
Partial pressures of respiratory gases in mm. Hg
|
Gas |
Oxygen |
Carbon dioxide |
Nitrogen |
|
Inspired air |
158 |
0.3 |
596 |
|
Alveolar air |
100-105 |
40 |
573 |
|
Venous blood |
40 |
46 |
573 |
|
Arterial blood |
95-100 |
40 |
573 |
|
Expired air |
116 |
32 |
565 |
|
Tissue cells |
20-40 |
45-52 |
- |
Composition of three samples of air
|
Gas |
Oxygen |
Carbon dioxide |
Nitrogen |
Water |
|
Inspired air |
20.84% |
0.04% |
78.62% |
0.5% |
|
Expired air |
15.70% |
4.00% |
74.50% |
6.2% |
|
Alveolar air |
13.6% |
5.3% |
74.9% |
6.2% |
|
Gain/loss % |
Gain 5.14% |
Loss 3.96% |
Gain 4.12% |
Loss 5.7% |
Exchange of gases in lungs can be divided into two steps -
Uptake of \[{{O}_{2}}\] by blood in lung : The \[{{P}_{{{O}_{2}}}}\] (partial pressure of oxygen) of the alveolar air is higher than the \[{{P}_{{{O}_{2}}}}\] of blood in alveolar capillaries. Due to a \[{{P}_{{{O}_{2}}}}\] difference between air and blood, oxygen diffuses rapidly from the alveolar air into the blood of alveolar capillaries.
Release of \[C{{O}_{2}}\] by the blood : The \[{{P}_{C{{O}_{2}}}}\] (partial pressure of carbon dioxide) of blood reaching the alveolar capillaries is higher than the \[{{P}_{C{{O}_{2}}}}\] of alveolar air. Therefore, carbon dioxide diffuses from the blood of alveolar capillaries into the alveolar air.
(ii) Exchange of gases in tissues : In the tissues, exchange of gases occurs between the blood and the tissue cells. This exchange occurs via tissue fluid that bathes the tissue cells. The blood reaching the tissue capillaries has \[{{P}_{{{O}_{2}}}}\] higher than that in the tissue cells and \[{{P}_{C{{O}_{2}}}}\] lower than that in the tissue cells. The tissue cells constantly use oxygen in oxidation that produces carbon dioxide. Therefore, they always have lower\[{{P}_{{{O}_{2}}}}\] and higher \[{{P}_{C{{O}_{2}}}}\]than the blood coming to them. Because of \[{{P}_{{{O}_{2}}}}\]and \[{{P}_{C{{O}_{2}}}}\]differences between blood and tissue cells, oxygen separates from oxyhaemoglobin and diffuses from the blood into the tissue fluid and hence in to the tissue cells; and carbon dioxide diffuses from the tissue cells in to the tissue fluid and thence in to the blood in the tissue capillaries. Gases mostly diffuse through the tissue fluid as such, only small amounts dissolve in it.
Exchange of gases in the tissues that lowers the \[{{P}_{{{O}_{2}}}}\]of the blood and raises its \[{{P}_{C{{O}_{2}}}}\]is called internal respiration. The blood deoxygenated by this respiration returns to the right side of the heart that sends it to the lungs for reoxygenation.
(3) Transport of gases : Blood carries \[{{O}_{2}}\] from respiratory organs to the tissue cells for oxidation and \[C{{O}_{2}}\] from tissue cells to respiratory organs for elimination. Blood should be slightly alkaline to help the transport of \[{{O}_{2}}\] and \[C{{O}_{2}}\] properly.
(i) Transport of oxygen : Lung contains atmospheric air. From the lung O2 diffuses into the blood. The blood transport O2 from the lung to the cells. This is called oxygen transport. \[{{O}_{2}}\] is carried in the blood in three forms –
(a) In physical solution : 100 ml. oxygenated blood contains 20 ml(0.3 ml dissolved in plasma and 19.7 ml bound to Hb) of oxygen. \[2-3%\] oxygen is transported in form of physical solution. Thus 0.3 ml to 0.6 ml. \[{{O}_{2}}\] is in physical solution form in 100 ml of blood.
(b) As oxyhaemoglobin \[(Hb{{O}_{2}})\] : Most of \[{{O}_{2}}\] is transported in form of oxyhaemoglobin. 98.5% in the form of \[Hb{{O}_{2}},\] 1.5% is carried in the dissolved state in watery blood plasma. \[{{O}_{2}}\] is transported in form of oxyhaemoglobin.
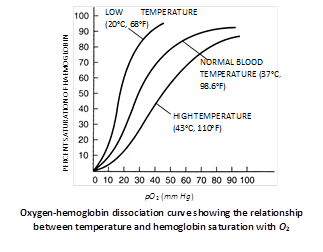
Oxygen-haemoglobin dissociation curve
When a graph is plotted between percent saturation of haemoglobin and oxygen tension, a curve is obtained termed as \[{{O}_{2}}-Hb\]dissociation curve. Oxygen\[-Hb\] dissociation curve is sigmoid shaped-or S shaped. This sigmoid shaped curve is characteristic for Hb.
Body tissue obtain oxygen from oxyhaemoglobin because of its dissociation caused by low \[{{O}_{2}}\] and high \[C{{O}_{2}}\]concentration. Under a given oxygen concentration in blood, dissociation of oxyhaemoglobin will increase if pH of blood falls. When partial pressure of \[C{{O}_{2}}\]rises (blood pH decreases), dissociation curve of oxyhaemoglobin at 37°C shift to right. Effect of high temperature and low pH (high \[PC{{O}_{2}}\]) are similer. \[{{P}_{50}}\]indicates the oxygen concentration at which 50% haemoglobin of blood is saturated with \[{{O}_{2}}.\]
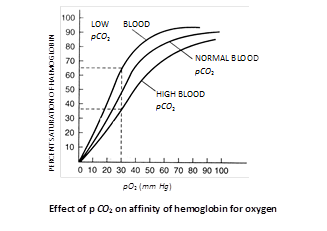
Bohr’s effect : Hb-\[{{O}_{2}}\] dissociation curve shifts to right when \[C{{O}_{2}}\] tension in blood is high. Bohr discovered this effect in 1904. Bohr effect is the effect of \[C{{O}_{2}}\]on oxyhaemoglobin. Deoxygenation of oxygaemoglobin is directly proportional to blood pCO2. Extent of Bohr’s effect depends upon the tension of \[C{{O}_{2}}\] in blood only. \[C{{O}_{2}}\] of tissue fluid and alveoli does not exert Bohr’s effect. During exercise muscles need more \[{{O}_{2}}\] and want to remove \[C{{O}_{2}}\] which has high production. Because of pressure gradient \[C{{O}_{2}}\] moves from tissues fluid to capillary blood\[\to \]Exert Bohr’s effect \[\to \,\,{{O}_{2}}\] release is hastened from \[Hb-~{{O}_{2}}\,\,i.e.\,\,Hb-{{O}_{2}}\]curve shifts to right.
Haemoglobin : Oxygen carrier or respiratory pigment in vertebrates blood is haemoglobin. Hb molecule is made of two components haem and globin. Globin part is globulin protein which is made of four polypeptide chain, two \[\alpha \] chains (141 amino acid) and two b chains (146 amino acid). Thus total no. of amino acid in Hb 574. Haem is iron containing compound and belongs to the class of compound called protoporphyrins. Hb in RBC synthesized before loss of nucleus. Iron of Hb is in ferrous state \[(F{{e}^{++}})\] and even after the combination with \[{{O}_{2}}\] it remains ferrous. One Hb molecule has 4 haem molecules. Each haem is associated without polypeptide chain. Each Hb molecule can combine with one molecule (2 atoms) of oxygen. Thus each molecule of Hb combines 4 molecules of \[{{O}_{2}}.\]
Myoglobin : It is chemically and functionally similar to Hb. It is made up of one polypeptide chain (153 amino acids) attached with on haem group. \[{{P}_{50}}\] value for myoglobin is 5 mm Hg. This indicates that myoglobin release oxygen less readily than Hb. It is found in muscles. It acts as a store house for \[{{O}_{2}}.\] An average man can store about 1.5 litre oxygen in myoglobin. Hb-\[{{O}_{2}}\] dissociation curve for myoglobin is hyperbola.
(ii) Transport of \[C{{O}_{\mathbf{2}}}\]: Transportation of \[C{{O}_{2}}\] by blood is mush easier due to its high (20 times that of \[{{O}_{2}}\]) solubility in water. Blood can carry upto 50% or 60% of CO2 by volume, but normally about 4 ml of CO2 on an average is transported from tissue to the lungs in each 100 ml of blood in man. With 5 litres of cardiac output per minute, the blood thus transports about 200 to 220 ml of \[C{{O}_{2}}\] each minute. Obviously, this is the rate at which \[C{{O}_{2}}\] is produced and released into tissue fluids by cells, and at which it diffuses out into alveolar air from pulmonary arterial blood. The blood transports this \[C{{O}_{2}}\] in three ways.
(a) In dissolved state : Deoxygenated (\[HC{{O}^{}}_{3}\] is 45 to 46 mm Hg) and oxygenated (\[PC{{O}_{2}}\]is 40 mm Hg) bloods respectively carry about 2.7 and 2.4 ml of \[C{{O}_{2}}\] per 100 ml of blood in dissolved state in plasma (= in solution with plasma). Thus, about 0.3 (2.7 minus 2.4) ml of \[C{{O}_{2}}\] is transported by each 100 ml. of blood in dissolved state in plasma. This is about 7% of all the \[C{{O}_{2}}\] transported by blood from tissues to the lungs.
(b) In the form of bicarbonate ions : Most of the \[C{{O}_{2}}\] that dissolved in blood plasma reacts with water, forming carbonic acid - \[C{{O}_{2}}+{{H}_{2}}O\rightleftharpoons {{H}_{2}}C{{O}_{3}}\] (carbonic acid)
This reaction is very slow in plasma, but occurs very rapidly inside RBCs, because an enzyme, carbonic anhydrase, present in RBCs, accelerates its rate about 5000 times. That is why, about 70% of the \[C{{O}_{2}}\] (about 2.5 ml per 100 ml of blood), received by blood from the tissues, immediately enters into RBCs and hydrated to carbonic acid. Almost as rapidly as formed, all carbonic acid of RBCs dissociates into hydrogen and bicarbonate ions (\[{{H}^{+}}\]and\[HC{{O}^{}}_{3}\]). The hydrogen ions mostly combine with heamoglobin for keeping the pH of blood. (7.4) in steady state, because haemoglobin is a powerful acid base buffer. Being quite diffusible, the bicarbonate ions, on the other hand, diffuse from RBCs into the plasma. To maintain electrostatic neutrality of plasma, many chloride ions, in turn, diffuse from plasma into the RBCs. Obviously, the chloride contents of RBCs increase when oxygenated blood becomes deoxygenated. This is termed “chloride or Hamburger shift”.
Sequence of events : From tissues \[C{{O}_{2}}\] enters in plasma\[\to \]a small fraction of \[C{{O}_{2}}\] is dissolved in plasma\[\to \]rest of \[C{{O}_{2}}\] enters into the RBC\[\to \]within RBC \[C{{O}_{2}}\] combines with \[{{H}_{2}}O\] in presence of enzyme carbonic anhydrase and forms \[{{H}_{2}}C{{O}_{3}}\to {{H}_{2}}C{{O}_{3}}\] splits into \[{{H}^{+}}\] and \[HCO_{3}^{-}\to \]most of the\[HCO_{3}^{-}\] comes out of RBC and enters in plasma and form \[NaHC{{O}_{3}},\] small fraction stays back within the RBC to form \[KHC{{O}_{3}}\] and \[{{H}^{+}}\] combine with Hb to form reduced haemoglobin H.Hb.
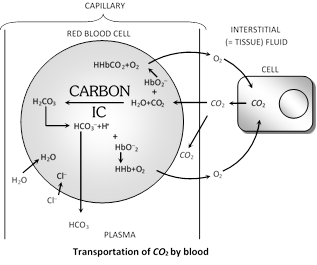
(c) In the form of carbamino compounds : In addition to reacting with water, \[C{{O}_{2}}\] also directly and reversibly reacts with haemoglobin, loosely binding with it and forming an unstable compound, called carbaminohaemoglobin (\[(C{{O}_{2}}HHb).\]). It also similarly forms loose bonds with some plasma proteins. It is estimated that about 23% of the \[C{{O}_{2}}\] (1 ml per 100 ml of blood), collected from cells through tissue fluids, is transported by blood in this form.
Transformation of \[C{{O}_{2}}\] in various forms
| Transformation forms of \[C{{O}_{2}}\] | Transported quantity |
|
\[C{{O}_{2}}\] |
7 % (0.3 ml/100ml of blood) |
|
\[HHbC{{O}_{2}}\] |
23% (1ml/100 ml of blood) |
|
\[HC{{O}_{3}}^{}\] |
70% (2.5 ml/100 ml of blood) |
Haldane effect and \[C{{O}_{2}}\] diffusion into the alveoli : Whereas the Bohr effect promotes \[{{O}_{2}}\] transport, the Haldane effect is important in promoting \[C{{O}_{2}}\] transport. The Haldane effect results from the simple fact that oxyhaemoglobin behaves as a strong acid. This in turn, displaces \[C{{O}_{2}}\] from the blood in two ways.
(1) Due to its increased acidity, the haemoglobin loses its capacity to combine with \[C{{O}_{2}}.\]Hence all carbamino haemoglobin dissociates to release its \[C{{O}_{2}}.\]
(2) Secondly, the highly acidic oxyhaemoglobin releases an excess of \[{{H}^{+}}\] which bind with bicarbonate ions \[(HC{{O}_{3}}^{}),\] forming carbonic acid. The latter soon dissociates into \[{{H}_{2}}O\] and \[C{{O}_{2}}.\] This \[C{{O}_{2}}\]diffuses into the alveoli.
Thus, in the lung, the haldane effect, increases release of \[C{{O}_{2}}\] because of \[{{O}_{2}}\] uptake by haemoglobin. In the tissues a reverse process occurs. The Haldane effect increases \[C{{O}_{2}}\]uptake because of removal of \[{{O}_{2}}\] from haemoglobin.
Control of breathing
Respiratory rhythm is controlled by nervous system. Inspiratory and expiratory centres are jointly called rhythmicity centres. Inspiratory centre is dominant over expiratory centre. When pneumotaxic is stimulated respiration rate increases inspiration as well as expiration is shortened. Respiratory movements are under control of medulla oblongata.
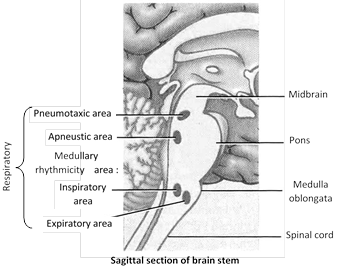
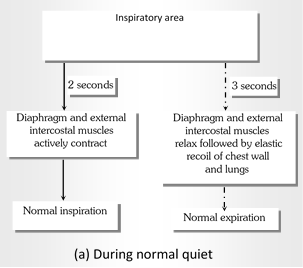
For the control of respiration following respiratory centres are found in hind brain
|
Type of centre |
Location |
Function |
|
Inspiratory centre |
Medulla oblongata |
Inspiration (2 second active condition). |
|
Respiratory centre |
Medulla oblongata |
Expiration (3 second inactive condition) |
|
Apneustic centre |
Pons |
Slow and deep inspiration |
|
Pneumotaxic centre |
Pons |
Control other centres and produce normal quite breathing |
|
Gasping centre |
Pons |
Sudden and shallow respiration |
(1) Chemical control : This includes \[C{{O}_{2}},\,\,{{O}_{2}}\] and \[{{H}^{+}}\]conc. of blood for detection of concentration of \[{{O}_{2}},\,\,C{{O}_{2}}\] and \[{{H}^{+}}\] ions in blood two types of receptors are found. These receptors are called chemoreceptor.
Peripheral chemoreceptor : These include two sets - Carotid body is present in the wall of the left and the right common carotid arteries and aortic bodies is present in the arch of aorta. They are placed in the vascular endothelium and come in contact with the blood. When \[P{{O}_{2}}\]decreases or increases in arterial blood, these receptors are stimulated and send impulses to respiratory centre to respectively increases or decreases the rate intensity of inspiratory signals.
(2) Central chemoreceptors : These are present on ventral surface of medulla. Cells of these centres are bathed in brain tissue fluid. They are in close vicinity of CSF. In brain tissue fluid as well as in CSF the\[C{{O}_{2}}\]is converted into \[{{H}_{2}}C{{O}_{3}}\to {{H}_{2}}C{{O}_{3}}\,\,{{H}^{+}}+HCO_{3}^{-}\to {{H}^{+}}\] ions are liberated \[\to {{H}^{+}}\] ions stimulate the central chemoreceptor (C.C) cell \[\to \] stimulation from C.C goes to respiratory centre \[\to \]Respiration stimulate.
(3) Effect of different gases
(i) Effect of \[C{{O}_{2}}\]: Rise in tension of arterial \[C{{O}_{2}}\] or alveolar \[C{{O}_{2}}\] causes stimulation of respiration. Both the rate and depth of respiration increased. This leads to washing out of \[C{{O}_{2}}\] from body.
(ii) Effect of \[{{O}_{2}}\]: Fall of \[{{O}_{2}}\] concentration in inspired air causes stimulation of peripheral chemoreceptors neural impulse arise from peripheral chemoreceptors. These impulse gots respiratory centre and cause respiratory stimulation. Some factor which increase the respiratory rate.
You need to login to perform this action.
You will be redirected in
3 sec
