Physiology Of Excretion
Category : 11th Class
Major nitrogenous excretory substance in frog, rabbit and human is urea, i.e. these are ureotelic animals. The excretory physiology in these animals may be considered under two phases, viz urea synthesis and formation and excretion of urine.
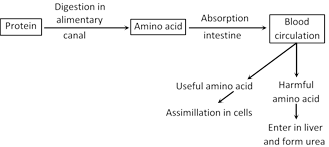
Synthesis of urea in liver : Urea is formed in liver by two processes.
(1) Deamination (2) Ornithine cycle
(1) Deamination : The amino acid is oxidised using oxygen. This result in removal of the amino group \[(N{{H}_{2}})\] and leaves pyruvic acid. the pyruvic acid can enter the Krebs cycle and be used as a source of energy in cell respiration. The amino group is converted to ammonia \[(N{{H}_{3}})\] during deamination. Deamination is also known as oxidative deamination.
\[\underset{\left( \text{Amino}\,\,\text{acid} \right)\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,}{\mathop{\begin{array}{*{35}{l}} C{{H}_{3}} \\ | \\ CH-N{{H}_{2}}+\frac{1}{2}{{O}_{2}} \\ | \\ COOH \\\end{array}\xrightarrow{{}}}}\,\underset{\left( \text{Pyruvic}\,\text{acid} \right)}{\mathop{\begin{array}{*{35}{l}} C{{H}_{3}} \\ | \\ CO+N{{H}_{3}} \\ | \\ COOH \\\end{array}}}\,\]
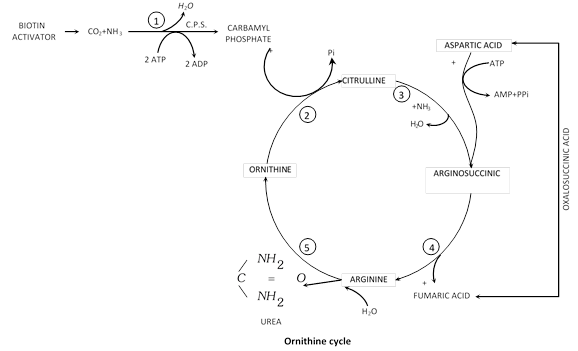
With the help of a number of enzymes and energy of A.T.P. two molecules of ammonia are combined with \[C{{O}_{2}}\] to form urea according to the ornithine cycle.
(2) Ornithine cycle (Kreb-Henseleit cycle) : In liver one molecule of \[C{{O}_{2}}\] is activated by biotin and combines with two molecules of \[N{{H}_{3}}\]in the presence of carbamyle phosphate synthatase enzyme (C.P.S.) and 2 ATP to form carbamyle phosphate and one molecule of \[{{H}_{2}}O\] release. Carbamyle phosphate react with ornithine and form citrulline. Citrulin combines with another molecule of ammonia and form arginine. Arginine is broken into urea and ornithine in the presence of an enzyme arginase and water.
\[2N{{H}_{3}}+C{{O}_{2}}\xrightarrow{\text{Arginase}}\underset{\text{(Urea)}}{\mathop{N{{H}_{2}}-CO-N{{H}_{2}}+{{H}_{2}}O}}\,\]
Liver cells, thus, continuously remove ammonia and some \[C{{O}_{2}}\] from blood and release urea into the blood. Kidneys continuously remove urea from the blood to excrete it in urine.
Urine formation : Urine formation occurs in the kidneys. It involves three processes glomerular filtration, reabsorption and tubular secretion.
(1) Ultra filtration (Starling’s hypothesis)
(i) It is passive process which takes place from the glomerulus into the Bowman's capsule. The glomerular epithelium has various micropores (diameter\[=50100\,\,nm\,\,or\text{ }0.050.1\,\,\mu m\]) which increase the rate of filtration.
(ii) The non colloidal part of the plasma as urea, water, glucose, salts, vitamin, minerals, nitrogenous waste are forced out from the glomerular capillaries into the Bowman's capsule by the high pressure of the blood in the glomerular capillaries. The pressure and resistence is high because the glomerular capillaries are narrower than the afferent renal arteries. Glomerular capillaries are about 50 times more permeable than capillaries elsewhere. Pressure highest in glomerular capillaries than in capillaries else where, produce more filtrate.
(iii) The effective filtration pressure that causes ultrafiltration is determined by three pressures.
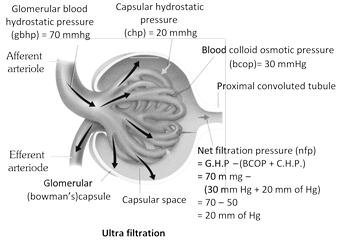
(a) Glomerular blood hydrostatic pressure (G.B.H.P.) : Hydrostatic pressure is force that a fluid under pressure exerts against the walls of its container.
\[G.B.H.P.=+70\,\,mm\text{ }Hg.\]
(b) Blood colloidal osmotic pressure (B.C.O.P) : The B.C.O.P. is the osmotic pressure created in the blood of glomerular capillaries due to plasma proteins albumin, globulin, and fibrinogen. It resists the filtration of fluid from the capillaries.
\[B.C.O.P.=30\,\,mm\text{ }Hg.\]
B.C.O.P. in other body capillaries is 25 mm Hg
(c) Capsular hydrostatic pressure (C.H.P) : C.H.P. is the pressure caused by fluid (filtrate) that reaches into Bowman's capsule and resists filtration.
\[C.H.P.=20\,\,mm\,\,Hg.\]
Effective filtration pressure (E.F.P.)/Net filtration pressure (N.F.P.) : E.F.P. is glomerular blood hydrostatic pressure minus the colloidal osmotic pressure of blood and capsular hydrostatic pressure.
\[E.F.P.=G.B.H.P.\text{ }(B.C.O.P.+C.H.P.)\]
\[=70\,\,mmg(30\,\,mmg\text{ }Hg+20\,\,mm\text{ }Hg)\]
\[=7050\]
\[E.F.P.=20\,\,mm\text{ }Hg\]
\[(N.O.F.P.)=B.C.O.P.+C.H.P.\]
\[=50\,\,mm\,\,Hg.\]
Glomerular filtrate : The plasma fluid that filters out from glomerular capillaries into Bowman's capsule of nephrons is called glomerular filtrate. It is a non colloidal part and possess urea, water, glucose, amino acid, vitamins, fatty acid, uric acid, creatin, creatinine, toxins, salts etc.
R.B.Cs, W.B.Cs, platelets and plasma proteins are the colloidal part of the blood and do not filtered out from glomerulus. Glomerular filtrate is isotonic to blood plasma.
Glomerular filtrate or Nephric filtrate
= Blood – (Blood cells + Plasma protein)
or
= Blood – (R.B.Cs + W.B.Cs + platelets + plasma protein)
or
\[=PlasmaProtein\]
Glomerular filtration rate (G.F.R.) : G.F.R. is the amount of filtrate formed per minute in all nephrons of the paired kidney. There is a sexual difference. In male the rate is \[120125\,\,ml/min,\] in female it is \[110\,\,ml/min.\text{ }G.F.R.\] is affected by volume of circulating blood, neural activity, stretch response to pressure of the wall of the arteriole.
180 litre of filtrate is formed per day, out of it, only 1.5 litre of urine is produced per day which is 0.8% of the total filtrate.
Renal plasma flow : About 1250 ml (25% of cardiac output or total blood) blood circulates through kidneys each minute and of this blood, about 670 ml is the plasma. The latter is called the renal plasma flow (R.P.F.)
\[R.P.F.=670\,\,ml.\]
Filtration fraction : This is the ratio of G.F.R. to R.P.F., and it is called filtration fraction.
Filtration fraction \[=\frac{G.F.R.}{R.P.F.}=\frac{120}{670}=0.17\]
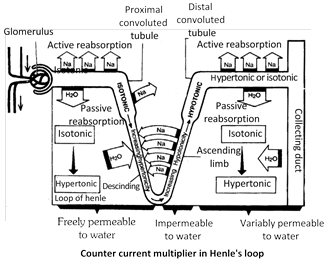
(2) Selective reabsorption : Discovered by Richard and supporters.
Proximal convoluted tubule : P.C.T. is the pivotal site for reabsorption. Glucose, amino acid and \[N{{a}^{+}},{{K}^{+}}\] ions are reabsorbed by active transport. \[C{{l}^{-}}\] are reabsorbed by passive transport following the positively charged ions.
Active uptake of ions reduces the concentration of the filtrate and an equivalent amount of water passes into the peritubular capillaries by osmosis. (Here 80% water is reabsorbed by passive transport. It is also known as obligatory water reabsorption). Most of the important buffer bicarbonate \[(HCO_{3}^{-})\] is also reabsorbed from the filtrate. P.C.T. absorb nearly \[8090\,\,%\] of filtered bicarbonate. Some urea is reabsorbed by diffusion. The rest remain in the filtrate for removed in the urine.
Henle's loop : See counter current mechanism.
Distal convoluted tubule : When the level of plasma water falls, the posterior pituitary lobe release the antidiuretic hormone (ADH) which increases the permeablity of the distal convoluted tubule and the collecting duct to water. Water is reabsorbed from the filtrate by osmosis and a reduced amount of concentrated urine is produced (Here 13% water is reabsorbed by facultative reabsorption)
The distal convoluted tubule and the collecting duct actively reabsorbed sodium from the filtrate under influence of the adrenal hormone aldosteron which makes their walls permeable to ions. The reabsorption of \[N{{a}^{+}}\] brings about the uptake of an osmotically equivalent amount of water. But duct of Bellini is relatively impermeable to water. Bicarbonate ions are also reabsorbed in D.C.T.
(3) Tubular secretion : It occurs as under -
(i) Creatinine, hippuric acid and foreign substances (pigments, drugs including penicillin) are actively secreted into the filtrate in the PCT from the interstitial fluid. Hydrogen ions and ammonia \[(N{{H}_{3}})\] are also secreted into the PCT.
(ii) Potassium, hydrogen, \[NH_{4}^{+}\] and \[HCO_{3}^{-}\] ions are secreted by active transport, into the filtrate in the DCT.
(iii) Urea enters the filtrate by diffusion in the thin region of the ascending limb of Henle's loop.
Removal of \[{{H}^{+}}\] and \[NH_{4}^{+}\] from the blood in the PCT and DCT helps to maintain the pH of the blood between 6 to 8. Any variation from this range is dangerous.
Tubular secretion probably plays only a minor role in the function of human kidneys, but in animals, such as marine fish and desert amphibians which lack glomeruli and Bowman's capsules, tubular secretion is the only mode of excretion. When the blood pressure, and consequently the filtration pressure, drop below a certain level, filtration stops and urine is formed by tubular secretion only.
High threshold substances : Such substances are absorbed almost all. Example - Sugar, amino acids, vitamins, \[HC{{O}_{3}}^{}\]and \[N{{a}^{+}}\] etc.
Low threshold substances : They are absorbed in low concentration. Example - Urea, phosphate, uric acid, \[{{H}^{+}},\text{ }{{K}^{+}}.\]
Non threshold substances : They are not reabsorbed. Example - Creatinine and hippuric acid.
Diuretic substances : Normally, the amount of urine formed depends on the intake of water, dietary constituents, environmental temperature, mental and physiological states of the person. However, there are some substances which increase the volume of urine to be excreted, these substances are called diuretic substances. Exmaple - Tea, Coffee, alcohol etc.
Mechanism of urine concentration (Counter current mechanism of urine concentration) : Mammals form hypertonic urine. The urine is made hypertonic with the help of counter current multiplier system. This process takes place in the Henle's loop and vasa recta and it involves mainly \[N{{a}^{+}}\] and \[C{{l}^{-}}.\]In P.C.T. urine is isotonic. The descending limb of loop of Henle is permeable to water. Its surrounding tissue fluid is hypertonic. Hence, the water moves out and the \[N{{a}^{+}}\]and \[C{{l}^{-}}\] moves in the descending limb by passive transport. Therefore, the filtrate in the descending limb finally becomes hypertonic.
The ascending limb of the Henle's loop is impermeable to the water. The\[N{{a}^{+}}\]and \[C{{l}^{-}}\] moves out by active transport. Hence the filtrate finally becomes hypotonic. The\[N{{a}^{+}}\]and \[C{{l}^{-}}\] re-enter into the descending limb of the Henle's loop. The collecting duct always passes through the hypertonic tissue fluid. Hence, water comes out osmotically making the filtrate hypertonic. Now in collecting duct glomerular filtrate is known as urine. Term urine first time use in collecting duct.
Summary of events occurring in a nephron
|
S.No. |
Materials transferred in traces |
Nephron region |
Process involved |
Mechanism |
|
1. |
Glucose, Amino acids, protein albumin, Vitamins, Hormones, \[N{{a}^{+}},{{K}^{+}},M{{g}^{2+}},C{{a}^{+2}},\]\[{{H}_{2}}O,HC{{O}_{3}}^{},\] Urea, Uric Acid, Creatinine, Ketone Bodies. |
Bowman's capsule |
Glomerular filtration |
Ultrafiltration |
|
2. |
Glucose, Amino Acids, Hormones, Vitamins, \[N{{a}^{+}},{{K}^{+}},M{{g}^{2+}},C{{a}^{+2}}\] |
Proximal convoluted tubule |
Reabsorption |
Active transport |
|
3. |
\[C{{l}^{}}\] |
Proximal convoluted tubule |
Reabsorption |
Passive transport |
|
4. |
Water |
Proximal convoluted tubule |
Reabsorption |
Osmosis |
|
5. |
Urea |
Proximal convoluted tubule |
Reabsorption |
Diffusion |
|
6. |
\[{{H}_{2}}O\] |
Narrow region of descending limb of Henle's loop |
Reabsorption |
Osmosis |
|
7. |
\[N{{a}^{+}},{{K}^{+}},M{{g}^{+2}},C{{a}^{+2}},C{{l}^{}}\] |
Narrow region of ascending limb of Henle's loop |
Reabsorption |
Diffusion |
|
8. |
Inorganic ions as above |
Wide part of ascending limb of Henle's loop |
Reabsorption |
Active transport |
|
9. |
\[{{H}_{2}}O\] |
Distal convoluted tubule, collecting tubule, collecting duct |
Reabsorption with ADH Help |
Osmosis |
|
10. |
\[N{{a}^{+}}\] |
Distal convoluted tubule, collecting tubule, collecting duct |
Reabsorption with aldosterone help reabsorption secretion |
Active transport |
|
11. |
Urea |
Last part of collecting duct |
Reabsorption with aldosterone help reabsorption secretion |
Diffusion |
|
12. |
Creatinine, Hippuric Acid, Foreign substances |
Proximal convoluted tubule |
Reabsorption with aldosterone help reabsorption secretion |
Active transport |
|
13. |
\[{{K}^{+}},{{H}^{+}}\] |
Distal convoluted tubule |
Reabsorption with aldosterone help reabsorption secretion |
Active transport |
|
14. |
\[N{{H}_{3}}\] |
Distal convoluted tubule |
Reabsorption with aldosterone help reabsorption secretion |
Diffusion |
|
15. |
Urea |
Ascending limb of Henle's loop (Thin part) |
Reabsorption with aldosterone help reabsorption secretion |
Diffusion |
You need to login to perform this action.
You will be redirected in
3 sec
