Category : 11th Class
The gonads are the sex glands, the testes and the ovary. Testes is the male gonad and ovary is the female gonads. Besides producing gametes, the gonads secrete sex hormones from the onset of puberty (sexual maturity) to control the reproductive organs and sexual behaviour.
The sex hormone were discovered by Adolf Butenononal in 1929 and 1931. He won the 1939 Nobel prize jointly with Leopold Ruzicka.
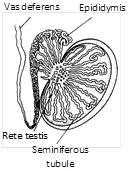
Testes
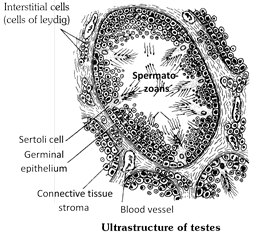
Location and structure : In testes between the siminiferous tubules, special types of cells are present called interstitial cells or cells of leydig. These cells secrete male hormones (androgens) derived from cholesterol. The main androgen is testosterone other less important androgens include androstenedione and dehydroepiandrosterone (DHEA). It is a masculinizing hormone. From puberty to the age of about twenty year i.e. adolescence or the period of sexual maturation or attainment of adult hood.
Function
(1) It stimulates the male reproductive system to grow to full size and become functional.
(2) It stimulates the formation of sperms (spermatogenesis) in the seminiferous tubules.
(3) It stimulates the development of male accessory sex characters such as hair on the face (beard and moustaches), growth and distribution of hair on the body, thickening of skin, deepening of voice, enlargement of larynx, broadening of shoulders, Narrow lips enlarged and stronger bones and muscles. It also maintains these characters.
(4) It also determines the male sexual behaviour sex urge, aggressive behaviour.
(5) Under its effect protein anabolism increases. (This function is obvious in the heavier muscle and bone mass of most men as compared to women).
(6) Grythropoisis in bone marrow increases.
(7) In brief, testosterone determines libido or sex drive. It is also required, together with the follicle stimulating hormone (FSH) of pituitary, for initiation and completion of spermatogenesis. All androgens are also secreted in traces from adrenal glands in both boys and girls.
(8) Increased sebaceous gland secretion.
Development of testis : Under the effect of chorionic gonadotropic hormone, secreted by placenta during pregnancy, the testes of eight to nine months old fetus start secreting testosterone. The latter regulates differentiation and development of urinogenital system, accessory genital organs and external genitalia in the embryo. During childhood i.e. from birth to puberty (age of 11 to 13 years), testes remain quiescent, so that androgens are not secreted. At puberty, the gonadotropic hormones (FSH and ICSH) of pituitary reactivate the testes which, therefore, start producing sperms and resume secreting androgens. Upto the age of about 40 years, androgens are secreted in sufficient amounts. There after, their secretion starts gradually declining, but the capability of reproduction still continues for many years.
Castration : Surgical removal of testes is called castration or orchidectomy. Castration, or deficient secretion of testosterone (hypogonadism) before puberty (due to congenital defects or injury to testes) retards growth of genitalia, muscles and bones, as well as, the development of sexual characteristics.
Castration or hypogonadism after puberty preserves the libido, but diminishes its overall efficiency (demasculinization). Muscular strength, hair growth, spermatogenesis, sex urge and potency sharply decline. sometimes, the person becomes impotent.
Castration is widely used in animal husbandry and domestication. Castrated cattle, horses and fowls are respectively called steers, geldings and capons. Castration makes these docile.
Primordial ovarian follicles are formed in the primitive ovaries of female fetuses as early as about 16 weeks of gestation, but these do not secrete hormones. Even in early childhood, upto the age of 7 or 8 years, ovaries remain quiescent. Thereafter, the pituitary starts secreting gonadotropins (FSH and LH) under whose influence puberty in girls sets in at about the age of 11 to 13 years; ovaries become active and menstrual cycle begins, so that the girls attain sexual maturity. Reproductive period, i.e., ovarian function and menstrual cycles in women normally cease at about the age of 45 to 55 years. This is called menopause. It usually results in a rise in urinary excretion of gonadotropins of the pituitary gland.
Ovarian hormone : Under the influence of FSH and LH. They secretes three female sex hormone, estrogen, progesteron and relaxin. They derived from cholesterol.
(1) Estrogens : These are secreted by the cells of the Graffian (ovarian) follicle surrounding the maturing ovum in the ovary. They stimulate the female reproductive tract to grow to full size and become functional. They also stimulate the differentiation of ova (oogenesis) in the ovary. They also stimulate the development of accessory sex characters such as enlargement of breasts; broadening of pelvis; growth of pubic and axillary hair; deposition of fat in the thighs, and onset of menstruation cycle. Graffian follicle cells are stimulated to secrete estrogens by luteinising hormone (LH) from the anterior lobe of the pituitary gland. Rise of blood-estrogens level above normal inhibits the secretion of LH from the anterior pituitary. This negative feedback prevents the oversecretion of estrogens.
(2) Progesterone : It is secreted by the corpus luteum. The latter is a yellowish body formed in the empty Graffian follicle after the release of the ovum. Its hormone suspends ovulation during pregnancy, fixes the foetus to the uterine wall, forms placenta, and controls the development of the foetus in the uterus. Ovulation, formation of corpus luteum and secretion of progesterone are stimulated by the luteinsing hormone (LH) from the anterior pituitary.
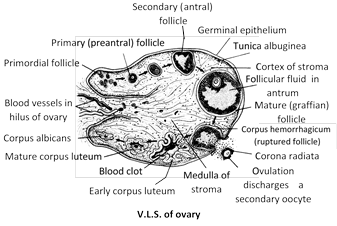
(3) Relaxin : It is produced by the corpus luteum at the end of the gestation period. It relaxes the cervix of the uterus and ligaments of the pelvic girdle for easy birth of the young one.
Regulation of ovarian hormone : Secretion of estrogens is regulated by the gonadotropins of pituitary. Undersecretion of estrogens (hypogonadism) before puberty due to congenital defects or damage to ovaries, causes female eunuchoidism. Accessory genitals and breasts remain underdeveloped, pelvis remains narrow and buttocks flat. Secondary sexual characteristics also do not develop. Hypogonadism in adulthood reduces fertility and disturbs menstrual cycles. Oversecretion (hypersecretion of hypergonadism) of estrogens also disturbs menstrual cycles and may even cause cancer.
Progesterone : Also called anti-abortion hormone.
Gravidex test : Involve testing of hcG of placenta in the urine to test the pregnancy.
Contraceptive pills : Contain less oestrogens and more progesterone so called combined pills. These check ovulation and so pregnancy in female.
Adiposogenital syndrome : Also called hypothalmic eunuchoidism characterized by hypogonadism in male caused by genetic inability of hypothalamus to secrete gonadotrophin releasing hormones.
Hormonal Contraception
Female contraception : As already described, gonads are stimulated to produces sex cells (gametes) and secrete sex hormones by the gonadotropic hormones (FSH and LH) of anterior pituitary. The anterior pituitary is, in turn, stimulated to secrete gonadotropins by the gonadotropin-releasing hormone (GnRH) of hypothalamus. In women, FSH promotes oogenesis and secretion of female hormones (estrogens). LH promotes ovulation, formation of corpus luteum and secretion of progesterone from it. A negative feedback regulation operates between GnRH and gonadotropins, on one hand, and between gonadotropins and female hormones on the other. Hence, high concentration of female hormones retards secretion of FSH, LH and GnRH due to which oogenesis does not occur, and pregnancy is out of question. Contraceptive pills of mixtures of estrogens and progesterone are more effective. The most popular contraceptive pills contain synthetic ethinyl estradiol and synthetic progesterone (e.g. norethindrone). In a modern method, a capsule of synthetic progesterone, like levonor gestrel, is implanted under the skin. The capsule serves for contraception for about five years.
Abortion is also now permissible in many countries to check population growth. Since progesterone is necessary to maintain early pregnancy, drugs, like mifepristone (RU-486), which inhibit the effects of progesterone are administered for abortion.
Male contraception : In men, LH stimulates cells of Leydig to secrete male hormones (androgens) of which testosterone is the principal hormone. Testosterone, in turn, inhibits LH secretion, but not FSH secretion by anterior pituitary. FSH and testosterone stimulate spermatogenesis. It has been found that large doses of testosterone can inhibit secretion of gonadotropin-release hormone (GnRH) by thalamic cells, thereby inhibiting secretion of both LH and FSH by pituitary. Hence systematically administered injections of testerone have been suggestes as a means of male contraception.
Recently, the cells of Sertoli in seminiferous have been found to secrete a protein factor named inhibin which directly inhibits secretion of FSH by pituitary. Hence, use of inhibin as a male contraceptive is now being explored.
You need to login to perform this action.
You will be redirected in
3 sec
