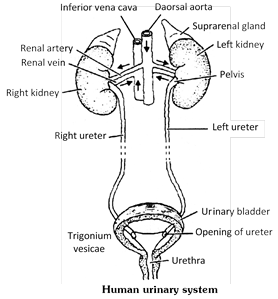
 The kidneys are covered by peritoneum on the front (ventral) side only. Thus, they are retroperitoneal. The right kidney is attached more anterior than the left in rabbit. This asymmetry is just the reverse of that found in man.
In man left kidney occurs at a slightly higher level than the right one, because right side has prominent right liver lobe. In rabbit the condition is little differ due to quadropedilism i.e. left kidney is in normal position while the right kidney shift ahead to provide place for stomach below it.
In mammals, the kidney is concavo convex. The center of concave inner surface is called as hilum or hilus which gives out a ureter. From this hilus surface the renal artery enters into the kidney, the renal vein comes out and the renal nerves enter into the kidney.
(i) Structure of kidney : The kidneys are metanephric in mammals. The kidney is divisible into two parts outer-cortex and inner-medulla. Three layers of tissue surround each kidney.
(a) The innermost, renal capsule made up of fibrous connective tissue.
(b) The intermediate layer, adipose capsule of fatty tissue.
(c) The outermost, renal fascia of dense connective tissue.
Renal pyramids or medullary pyramids : The medulla is subdivided into 8 to 18 conical masses - the renal pyramid, each having broad base towards the cortex and a narrow end called renal papilla towards the pelvis.
The kidneys are covered by peritoneum on the front (ventral) side only. Thus, they are retroperitoneal. The right kidney is attached more anterior than the left in rabbit. This asymmetry is just the reverse of that found in man.
In man left kidney occurs at a slightly higher level than the right one, because right side has prominent right liver lobe. In rabbit the condition is little differ due to quadropedilism i.e. left kidney is in normal position while the right kidney shift ahead to provide place for stomach below it.
In mammals, the kidney is concavo convex. The center of concave inner surface is called as hilum or hilus which gives out a ureter. From this hilus surface the renal artery enters into the kidney, the renal vein comes out and the renal nerves enter into the kidney.
(i) Structure of kidney : The kidneys are metanephric in mammals. The kidney is divisible into two parts outer-cortex and inner-medulla. Three layers of tissue surround each kidney.
(a) The innermost, renal capsule made up of fibrous connective tissue.
(b) The intermediate layer, adipose capsule of fatty tissue.
(c) The outermost, renal fascia of dense connective tissue.
Renal pyramids or medullary pyramids : The medulla is subdivided into 8 to 18 conical masses - the renal pyramid, each having broad base towards the cortex and a narrow end called renal papilla towards the pelvis.
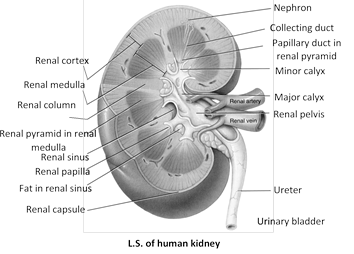 Path of urinary drainage : Collecting duct\[\to \]Papillary duct in renal pyramid\[\to \]Minor calyx\[\to \]Major calyx\[\to \]Renal pelvis\[\to \]Ureter\[\to \]Urinary bladder
Renal columns of bertini : Between the pyramids, the cortex extends into the medulla or renal columns of bertini.
Calyx : Each renal papilla projects into the cavity of a minor calyx, minor calyx join to form major calyx. The major calyx open into a wide funnel like structure, the pelvis. The latter leads into the ureter. In rabbit, the pelvis is unbranched hence, it is without calyx.
In frog ventral surface of each kidney has many ciliated funnels called nephrostomes. They drain wastes from body cavity (coelom) and connect to renal veins in frog or to uriniferous tubules in tadpoles.
(ii) Histology of kidney : Histologically a kidney is made of innumerable thin, long, much convoluted tubular units more...
Path of urinary drainage : Collecting duct\[\to \]Papillary duct in renal pyramid\[\to \]Minor calyx\[\to \]Major calyx\[\to \]Renal pelvis\[\to \]Ureter\[\to \]Urinary bladder
Renal columns of bertini : Between the pyramids, the cortex extends into the medulla or renal columns of bertini.
Calyx : Each renal papilla projects into the cavity of a minor calyx, minor calyx join to form major calyx. The major calyx open into a wide funnel like structure, the pelvis. The latter leads into the ureter. In rabbit, the pelvis is unbranched hence, it is without calyx.
In frog ventral surface of each kidney has many ciliated funnels called nephrostomes. They drain wastes from body cavity (coelom) and connect to renal veins in frog or to uriniferous tubules in tadpoles.
(ii) Histology of kidney : Histologically a kidney is made of innumerable thin, long, much convoluted tubular units more... 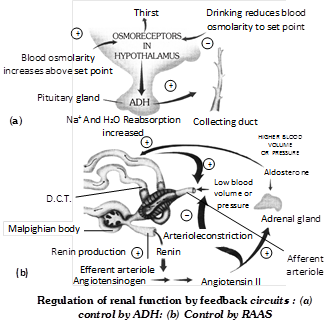 (3) Parathormone : The hormone increases blood \[C{{a}^{++}}\] (Hypercalcium) and decreases \[P{{O}_{4}}\] accordingly, it increases absorption of \[C{{a}^{+}},\]increases excretion of \[P{{O}_{4}}.\]
(4) Thyrocalcitonin : It increases excretion of \[C{{a}^{++}}\] in the kidney.
(5) Prostaglandin : The renal pyramids produce fatty acids of prostaglandins (P.G.) which participates in blood pressure regulation.
(6) Erythropoeitin : It is secreted by juxtaglomerular apparatus and plays an important role in erythropoeisis (blood production).
Differences between Rennin and Renin
(3) Parathormone : The hormone increases blood \[C{{a}^{++}}\] (Hypercalcium) and decreases \[P{{O}_{4}}\] accordingly, it increases absorption of \[C{{a}^{+}},\]increases excretion of \[P{{O}_{4}}.\]
(4) Thyrocalcitonin : It increases excretion of \[C{{a}^{++}}\] in the kidney.
(5) Prostaglandin : The renal pyramids produce fatty acids of prostaglandins (P.G.) which participates in blood pressure regulation.
(6) Erythropoeitin : It is secreted by juxtaglomerular apparatus and plays an important role in erythropoeisis (blood production).
Differences between Rennin and Renin
| S.No. | Rennin | Renin | ||||||||
| 1. | It is secreted by peptic (zymogen) cells of gastric glands into the stomach. | more...
The regulation of solute movement, and hence, water movement, which follows solutes by osmosis, is known as osmoregulation. Osmosis may be defined as a type of diffusion where the movement of water occurs selectively across a semipermeable membrane. It occurs whenever two solutions, separated by semipermeable membrane (the membrane that allows water molecules to pass but not the solutes) differ in total solute concentrations, or osmolarity. The total solute concentration is expressed as molarity or moles of solute per litre of solution. The unit of measurement for osmolarity is milliosmole per litre (mosm\[{{L}^{1}}\]). If two solutions have the same osmolarity, they are said to be isotonic. When two solutions differ in osmolarity, the solution with higher concentration of solute is called hypertonic, while the more dilute solution is called hypotonic. If a semipermeable membrane separates such solutions, the flow of water (osmosis) takes place from a hypotonic solution to a hypertonic one.
Osmoconformers are the animals that do not actively control the osmotic condition of their body fluids. They rather change the osmolarity of body fluids according to the osmolarity of the ambient medium. All marine invertebrates and some freshwater invertebrates are strictly osmoconformer. Osmoconformers show an excellent ability to tolerate a wide range of cellular osmotic environments.
Osmoregulators, on the other hand, are the animlas that maintain internal osmolarity, different from the surrounding medium in which they inhabit. Many aquatic invertebrates are strict or limited osmoregulators. Most vertebrates are strict osmoregulators, i.e. they maintain the composition of the body fluids within a narrow osmotic range. The notable exception, however, are the hagfish (Myxine sp., a marine cyclostome fish) and elasmobranch fish (sharks and rays).
Osmoregulators must either eliminate excess water if they are in hypotonic medium or continuously take in water to compensate for water loss if they are in a hypertonic situation. Therefore, osmoregulators have to spent energy to move water in or out and maintain osmotic gradients by manipulating solute concentrations in their body fluids.
Major nitrogenous excretory substance in frog, rabbit and human is urea, i.e. these are ureotelic animals. The excretory physiology in these animals may be considered under two phases, viz urea synthesis and formation and excretion of urine.
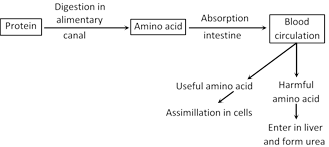 Synthesis of urea in liver : Urea is formed in liver by two processes.
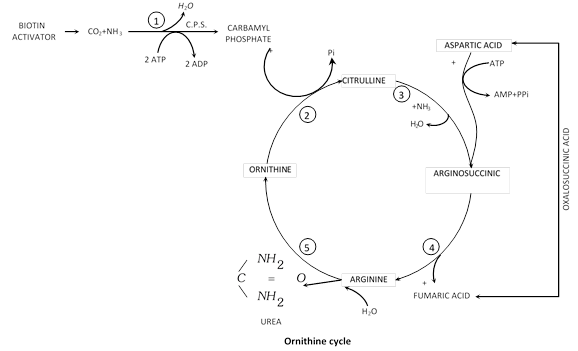
(1) Deamination (2) Ornithine cycle
(1) Deamination : The amino acid is oxidised using oxygen. This result in removal of the amino group \[(N{{H}_{2}})\] and leaves pyruvic acid. the pyruvic acid can enter the Krebs cycle and be used as a source of energy in cell respiration. The amino group is converted to ammonia \[(N{{H}_{3}})\] during deamination. Deamination is also known as oxidative deamination.
\[\underset{\left( \text{Amino}\,\,\text{acid} \right)\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,}{\mathop{\begin{array}{*{35}{l}} C{{H}_{3}} \\ | \\ CH-N{{H}_{2}}+\frac{1}{2}{{O}_{2}} \\ | \\ COOH \\\end{array}\xrightarrow{{}}}}\,\underset{\left( \text{Pyruvic}\,\text{acid} \right)}{\mathop{\begin{array}{*{35}{l}} C{{H}_{3}} \\ | \\ CO+N{{H}_{3}} \\ | \\ COOH \\\end{array}}}\,\]
With the help of a number of enzymes and energy of A.T.P. two molecules of ammonia are combined with \[C{{O}_{2}}\] to form urea according to the ornithine cycle.
(2) Ornithine cycle (Kreb-Henseleit cycle) : In liver one molecule of \[C{{O}_{2}}\] is activated by biotin and combines with two molecules of \[N{{H}_{3}}\]in the presence of carbamyle phosphate synthatase enzyme (C.P.S.) and 2 ATP to form carbamyle phosphate and one molecule of \[{{H}_{2}}O\] release. Carbamyle phosphate react with ornithine and form citrulline. Citrulin combines with another molecule of ammonia and form arginine. Arginine is broken into urea and ornithine in the presence of an enzyme arginase and water.
\[2N{{H}_{3}}+C{{O}_{2}}\xrightarrow{\text{Arginase}}\underset{\text{(Urea)}}{\mathop{N{{H}_{2}}-CO-N{{H}_{2}}+{{H}_{2}}O}}\,\]
Liver cells, thus, continuously remove ammonia and some \[C{{O}_{2}}\] from blood and release urea into the blood. Kidneys continuously remove urea from the blood to excrete it in urine.
Synthesis of urea in liver : Urea is formed in liver by two processes.
(1) Deamination (2) Ornithine cycle
(1) Deamination : The amino acid is oxidised using oxygen. This result in removal of the amino group \[(N{{H}_{2}})\] and leaves pyruvic acid. the pyruvic acid can enter the Krebs cycle and be used as a source of energy in cell respiration. The amino group is converted to ammonia \[(N{{H}_{3}})\] during deamination. Deamination is also known as oxidative deamination.
\[\underset{\left( \text{Amino}\,\,\text{acid} \right)\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,}{\mathop{\begin{array}{*{35}{l}} C{{H}_{3}} \\ | \\ CH-N{{H}_{2}}+\frac{1}{2}{{O}_{2}} \\ | \\ COOH \\\end{array}\xrightarrow{{}}}}\,\underset{\left( \text{Pyruvic}\,\text{acid} \right)}{\mathop{\begin{array}{*{35}{l}} C{{H}_{3}} \\ | \\ CO+N{{H}_{3}} \\ | \\ COOH \\\end{array}}}\,\]
With the help of a number of enzymes and energy of A.T.P. two molecules of ammonia are combined with \[C{{O}_{2}}\] to form urea according to the ornithine cycle.
(2) Ornithine cycle (Kreb-Henseleit cycle) : In liver one molecule of \[C{{O}_{2}}\] is activated by biotin and combines with two molecules of \[N{{H}_{3}}\]in the presence of carbamyle phosphate synthatase enzyme (C.P.S.) and 2 ATP to form carbamyle phosphate and one molecule of \[{{H}_{2}}O\] release. Carbamyle phosphate react with ornithine and form citrulline. Citrulin combines with another molecule of ammonia and form arginine. Arginine is broken into urea and ornithine in the presence of an enzyme arginase and water.
\[2N{{H}_{3}}+C{{O}_{2}}\xrightarrow{\text{Arginase}}\underset{\text{(Urea)}}{\mathop{N{{H}_{2}}-CO-N{{H}_{2}}+{{H}_{2}}O}}\,\]
Liver cells, thus, continuously remove ammonia and some \[C{{O}_{2}}\] from blood and release urea into the blood. Kidneys continuously remove urea from the blood to excrete it in urine.
 Urine formation : Urine formation occurs in the kidneys. It involves three processes glomerular filtration, reabsorption and tubular secretion.
(1) Ultra filtration (Starling’s hypothesis)
(i) It is passive process which takes place from the glomerulus into the Bowman's capsule. The glomerular epithelium has various micropores (diameter\[=50100\,\,nm\,\,or\text{ }0.050.1\,\,\mu m\]) which increase the rate of filtration.
(ii) The non colloidal part of the plasma as urea, water, glucose, salts, vitamin, minerals, nitrogenous waste are forced out from the glomerular capillaries into the Bowman's capsule by the high pressure of the blood in the glomerular capillaries. The pressure and resistence is high because the glomerular capillaries are narrower than the afferent renal arteries. Glomerular capillaries are about 50 times more permeable than capillaries elsewhere. Pressure highest in glomerular capillaries than in capillaries else where, produce more filtrate.
(iii) The effective filtration pressure that causes ultrafiltration is determined by three pressures.
Urine formation : Urine formation occurs in the kidneys. It involves three processes glomerular filtration, reabsorption and tubular secretion.
(1) Ultra filtration (Starling’s hypothesis)
(i) It is passive process which takes place from the glomerulus into the Bowman's capsule. The glomerular epithelium has various micropores (diameter\[=50100\,\,nm\,\,or\text{ }0.050.1\,\,\mu m\]) which increase the rate of filtration.
(ii) The non colloidal part of the plasma as urea, water, glucose, salts, vitamin, minerals, nitrogenous waste are forced out from the glomerular capillaries into the Bowman's capsule by the high pressure of the blood in the glomerular capillaries. The pressure and resistence is high because the glomerular capillaries are narrower than the afferent renal arteries. Glomerular capillaries are about 50 times more permeable than capillaries elsewhere. Pressure highest in glomerular capillaries than in capillaries else where, produce more filtrate.
(iii) The effective filtration pressure that causes ultrafiltration is determined by three pressures.
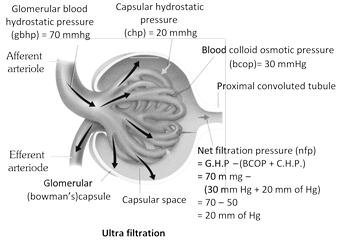 (a) Glomerular blood hydrostatic pressure (G.B.H.P.) : Hydrostatic pressure is force that a fluid under pressure exerts against the walls of its container.
\[G.B.H.P.=+70\,\,mm\text{ more...
(a) Glomerular blood hydrostatic pressure (G.B.H.P.) : Hydrostatic pressure is force that a fluid under pressure exerts against the walls of its container.
\[G.B.H.P.=+70\,\,mm\text{ more...
The fluid and dissolved waste substances excreted by the kidneys constitute urine.
Quantity : An adult man normally passes about 1 to 1.8 litres of urine in 24 hours. The volume of urine depends upon (i) the fluid intake, (ii) level of physical activity, (iii) type of food taken and (iv) environmental temperature increase urine output. Less fluid intake and profuse sweating due to heavy physical work and high temperature reduce urine output. Certain substances, such as tea, coffee and alcohol, increase urine output. These are said to be diuretic.
Physical properties : Urine is transparent yellowish fluid, but becomes turbid (cloudy) on standing, its colour depending on its concentration. Its colour is due to a pigment urochrome derived from the breakdown of haemoglobin from the worn-out RBCs. Colour of the urine is altered by certain materials taken such as beet, vitamin B complex and some drugs diseases. It is hypertonic to blood plasma. Its specific gravity ranges between 1.001 to 1.035, being slightly higher than that of water. Its pH is 6. It depends on the diet. High protein food and fruits increase acidity whereas vegetables increase alkalinity. Urine has a characteristic unpleasant odour. If allowed to stand, urea is degraded by bacteria to ammonia which imparts a strong smell to urine.
Chemical composition : Urine consists of water and organic and inorganic substances. Water alone forms about 95% of it, other substances form only 5%. The organic substances are mainly nitrogenous organic compounds include urea, uric acid, creatinine and hippuric acid. Of these, urea is the principal component of human urine. The non nitrogenous organic compounds include vitamin C, oxalic acid, phenolic substances include ammonia, and mineral salts such as chlorides, sulphates and phosphates of sodium, potassium, calcium and magnesium. Sodium chloride is the principal mineral salt of the urine. Urine also contains some other substances, such as pigments and drugs, and some epithelial cells, leucocytes, mucin, enzymes, and hormones.
Abnormal materials : Presence of proteins (albumins), bile salts, bile pigments, ketone bodies, blood, pus, microbes and more than a trace of glucose in the urine is pathological condition. Presence of glucose, protein, blood, ketone bodies and pus in the urine is called glucosurea, proteinuria, haematuria, ketonuria and pyuria respectively.
Renal threshold : A negligible amount of glucose is present in the urine. The highest concentration of a substances in the blood upto which it is fully reabsorbed from the glomerular filtrate is called its threshold. If its concentration in the blood exceeds its renal threshold, some of the filtered out substance is not reasborbed and is excreted in the urine. For example, the renal threshold of glucose is 180 mg. per 100 ml. of blood. If its blood level exceeds 180 mg., some of the filtered out glucose is not reabsorbed and is passed in urine.
Conduction of urine and Micturition : Urine is produced and drained continuously by the nephrons into the renal pelvis. From here, it is carried down the ureters by peristaltic waves into more...
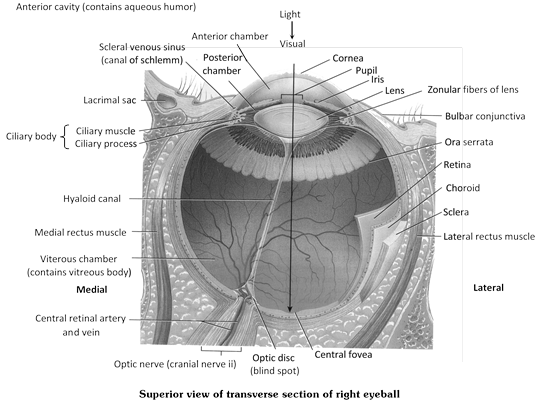
Human have binocular vision. The eye can discriminate colour, appraise length, width and depth visually and form true inverted image.
Structure of eye
The eyes are two in number and lodged in orbits (bony socket) of skull. The eye is a hollow, spherical organ, about 2.5 cm in diameter and about 6 to 8 gram in weight. It has two parts -
(1) Protective devices : Eye has four protective devices.
(i) Eye brows : The outwardly directed hair of the eyebrows carry the sweat and rain drops trickling down the forehead to the sides to prevent their falling into the eyes.
(ii) Eye lids (Palpebrae) : In man two eyelids are present, upper is movable. They are regularly closed at short intervals to clean the cornea. This is called blinking. In frog out of two upper eyelid is immovable and lower eyelid is movable. Nictitating membrane is present in frog which protect eye in water. Movement of nictitating membrane takes place by retractor bulbi. It becomes folded by levator bulbi.
A nonfunctional vestigeal nictitating membrane, called plica semilunaris, occurs in human eyes. It remains permanently retracted at the inner angle of each eye.
(iii) Eye lashes : The eyelids bear at the free edge a row of stiff hair, the eye lashes. These check the entry of dust particles, tiny insects and rain drops into the eyes.
 (iv) Eye glands
(a) Meibomian gland : The eye-lids bear at the free edge a row of meibomian gland that is modified sebaceous gland. (Act as a lumbricant).
(b) Lacrimal gland or Tear gland : It lies in the upper outer part of the orbit and secretes a slightly saline, watery fluid that contains a bacteriolytic enzyme named lysozyme. This secretion moistens the surface of the eyeball. The excess of this secretion passes through nasolacrimal duct. It is modified sweat gland.
(c) Harderian gland : Some aquatic mammals (whale) possess harderian gland which lubricate nictitating membrane. It is also found in frog and birds.
(d) Glands of zeis (zis) : These are modified sebaceous gland, found at base of hair follicle of eye lashes, pour lubricating fluid in hair follicle. Infection of these glands is sty.
(e) Glands of Moll : It is modified sweat gland and open into the follicles of eyelashes.
In human meibomian, lachrymal, Moll's glands, and zeis glands are present.
(v) Connective tissue : A layer of fatty connective tissue surrounds the eyeball. It serves as a soft shockproof pad.
(2) Eye ball : Eye ball is made up of 3 coats or tunic.
(i) Sclerotic layer (Fibrous tunica) : Outer most and opaque, fibrous and non-vascular layer easily seen as white of the eye. It is a coat of dense connective tissue made up of collagen fibers and fibroblasts. Sclera covers entire eye ball except cornea, gives shape to eye ball. Sclera in frog is cartilaginous.
(a) Cornea : In the more...
(iv) Eye glands
(a) Meibomian gland : The eye-lids bear at the free edge a row of meibomian gland that is modified sebaceous gland. (Act as a lumbricant).
(b) Lacrimal gland or Tear gland : It lies in the upper outer part of the orbit and secretes a slightly saline, watery fluid that contains a bacteriolytic enzyme named lysozyme. This secretion moistens the surface of the eyeball. The excess of this secretion passes through nasolacrimal duct. It is modified sweat gland.
(c) Harderian gland : Some aquatic mammals (whale) possess harderian gland which lubricate nictitating membrane. It is also found in frog and birds.
(d) Glands of zeis (zis) : These are modified sebaceous gland, found at base of hair follicle of eye lashes, pour lubricating fluid in hair follicle. Infection of these glands is sty.
(e) Glands of Moll : It is modified sweat gland and open into the follicles of eyelashes.
In human meibomian, lachrymal, Moll's glands, and zeis glands are present.
(v) Connective tissue : A layer of fatty connective tissue surrounds the eyeball. It serves as a soft shockproof pad.
(2) Eye ball : Eye ball is made up of 3 coats or tunic.
(i) Sclerotic layer (Fibrous tunica) : Outer most and opaque, fibrous and non-vascular layer easily seen as white of the eye. It is a coat of dense connective tissue made up of collagen fibers and fibroblasts. Sclera covers entire eye ball except cornea, gives shape to eye ball. Sclera in frog is cartilaginous.
(a) Cornea : In the more...
(1) Important tangoreceptor
(i) Merckel's corpuscles : Found in epidermis (stratum malphighi) of skin.
(ii) Merckel's disk : Found in epidermis (stratum malphighi) of skin.
(iii) Meissner's corpuscles : Present in skin around the base of hair and feather. These are sensitive for touch and pressure both.
(iv) Genital corpuscles : These are sensitive cells with nerve endings in skin around the genital organ.
(v) Grandey's corpuscles : Found in birds at the base of the beak. These are kidney shaped in structure.
(vi) Herbert corpuscles : Found in buccal cavity of birds.
(vii) Capsulated corpuscles : These are sensitive cells encapsulated and found in skin.
(viii) Paccinian corpuscles : Found in deep layer of dermis and sensitive to touch, pain and pressure.
(x) Golgi corpuscles and Mazzoni corpuscles : These are sensitive to touch and found in subcutaneous region.
(2) Important Olfactoreceptor
Jacobson's organ (Vomero-nasal organ) : It is concerned with smell. These were 1st appear in amphibians and well developed in snake, lizzard and sphenodon that is reptile. These are less developed in birds and mammal. Structure is blind sac like and lined by olfactory epithelium (Shneiderian membrane). Jacobsons organ is not found in rabbit. In man it is vestigeal organ. In human foetus Jacobson organ present. Jacobson organ also found in marsupiales, Rodents, and Insectivora.
(3) Important Thermoreceptor
(i) Krause end bulb : These are sensitive for temperature and pain and freidgo in nature. Found in lips, tongue, conjunctiva of eyes and corium of fingure.
(ii) Organ of Ruffeni : Sensitive to temperature and mainly related with heat.
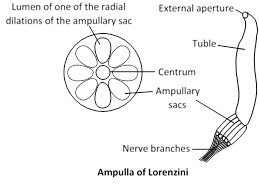
(iii) Ampulla of Lorenzini : Found in snout region of cartilagenous fishes these are helpful in detecting the temperature of water.
Also known as stato-acuostic organ. It is the receptor for balancing and hearing which is sensitive for gravity and sound waves. It is also sensitive in orientation of body. It is also known as mechano receptor because of it change mechanical energy of sound waves in to action potential.
Structure of Ear
Ear of mammal is divided in to 3 parts -
(1) External ear : It is made up of pinna and auditory meatus. Pinna is found in only mammals. Its upper rounded part is helix and lower is ear lobe. It is made up of adipose connective tissue and elastic cartilage and has ear muscles which are vestigeal in case of human beings. Pinna collect the sound waves and drive towards auditory meatus.
Auditory meatus is 25 mm. long canal lined by simple columnar epithelia and made up of fibro elastic cartilage. It possesses ceruminus gland which secrete cerumin (ear wax). Cerumin trap the dust particles and microbes.
Tympanic membrane : It is also called ear drum and present at the junction of auditory meatus and tympanic cavity.
(2) Middle ear : The cavity of middle ear is known as tympanic cavity which is enclosed by tympanic bulla bone of skull and filled with air. Middle ear separated from external ear by ear drum and from internal ear by thin bony portion or partition with two openings known as oval and round window.
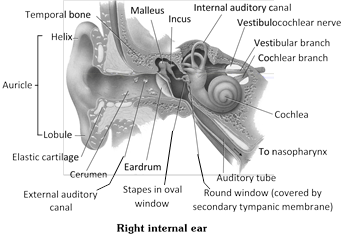 (i) Ear ossicle : A chain of three small, movable bones, the auditory or ear ossicles crosses the tympanic cavity. The outer ossicle is attached to the inner surface of the tympanic membrane.
(i) Ear ossicle : A chain of three small, movable bones, the auditory or ear ossicles crosses the tympanic cavity. The outer ossicle is attached to the inner surface of the tympanic membrane.
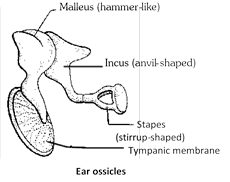 Ear ossicles
Ear ossicles
|