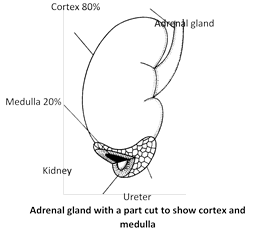
 Structure : Each adrenal is a small ( 5 cm long, 3 cm broad and 1 cm thick), triangular and yellowish cap like structure. Its weight in humans is about 3.5 to 5.09 gm. At birth Adrenal gland best developed. Each gland has two parts – Outer cortex and inner medulla.
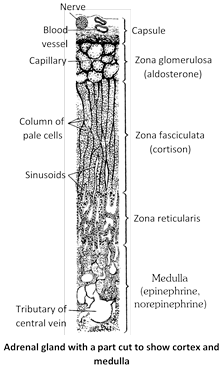
(1) Outer cortex : The cortex is derived from mesoderm and forms about 80% part of the gland. Cortex consists of fatty, cholesterol rich cells. These cells distinguish the cortex into three zones or regions.
(i) Zona glomerulosa : It is the outer part of the cortex (15% of the gland), which consists of small polyhedral cells. It secrets mineralocorticoids e.g., Aldosterone.
(ii) Zona fasciculata : It is the middle part of the cortex (50% of the gland). Which consists of large polyhedral cells. This part secrets gluco-corticoids. e.g., Cortison, Corticosterone.
(iii) Zona Reticularis : It is the inner part of the cortex (7% of the gland). In which the parallel cell cords of the zona fasciculata branched to form a loose anastomosing network. It secrets sex hormones.
(2) Inner medulla : The medulla is derived from ectoderm and forms about 20% part of the gland. Adrenal medulla is reddish brown in colour and colourless of rounded groups of short cords of relatively large and granular cells. These cells are modified postganglionic cells of sympathetic nervous system. These are called chromaffin cells or phaeochromocytes. Adrenal medulla secrets adrenalin and nor-adrenalin which are collectively called as catecholamines.
Hormones of adrenal cortex
About 20 steroids (steroidogenic) compounds have secreted from adrenal cortex. These are called adrenocorticoids (corticosteroids). Only few of them are biologically active as hormone. These hormones are steroid in nature. The later, however account about 80% of the secretion of adrenal cortex and are classified into three categories.
Structure : Each adrenal is a small ( 5 cm long, 3 cm broad and 1 cm thick), triangular and yellowish cap like structure. Its weight in humans is about 3.5 to 5.09 gm. At birth Adrenal gland best developed. Each gland has two parts – Outer cortex and inner medulla.
(1) Outer cortex : The cortex is derived from mesoderm and forms about 80% part of the gland. Cortex consists of fatty, cholesterol rich cells. These cells distinguish the cortex into three zones or regions.
(i) Zona glomerulosa : It is the outer part of the cortex (15% of the gland), which consists of small polyhedral cells. It secrets mineralocorticoids e.g., Aldosterone.
(ii) Zona fasciculata : It is the middle part of the cortex (50% of the gland). Which consists of large polyhedral cells. This part secrets gluco-corticoids. e.g., Cortison, Corticosterone.
(iii) Zona Reticularis : It is the inner part of the cortex (7% of the gland). In which the parallel cell cords of the zona fasciculata branched to form a loose anastomosing network. It secrets sex hormones.
(2) Inner medulla : The medulla is derived from ectoderm and forms about 20% part of the gland. Adrenal medulla is reddish brown in colour and colourless of rounded groups of short cords of relatively large and granular cells. These cells are modified postganglionic cells of sympathetic nervous system. These are called chromaffin cells or phaeochromocytes. Adrenal medulla secrets adrenalin and nor-adrenalin which are collectively called as catecholamines.
Hormones of adrenal cortex
About 20 steroids (steroidogenic) compounds have secreted from adrenal cortex. These are called adrenocorticoids (corticosteroids). Only few of them are biologically active as hormone. These hormones are steroid in nature. The later, however account about 80% of the secretion of adrenal cortex and are classified into three categories.
 (1) Mineralo-corticoids : The principal mineralocorticoid is aldosterone. It is also called salt-retaining hormone. It promotes reabsorption of sodium ions from kidney and excretion of potassium ions in urine. It also reabsorb Cl– ions from kidney. Thus aldosterone has a important contribution in homeostasis by controling osmatic pressure of ECF (Extra cellular fluid).
Remember that doctors administer saline drip to the patients who lose excessive water and salts due to diarrhoea, cholera, etc. Aldosterone also helps in maintaining acid-base equilibrium and blood pH (7.35) by promoting reabsorption of \[HC{{O}^{}}_{3}\] and regulating excretion of \[{{H}^{+}}\]by kidneys. It also promotes absorption of water and salt in intestine, mainly in colon. The Renin-angiotensin-aldosterone or RAA pathway controls more...
(1) Mineralo-corticoids : The principal mineralocorticoid is aldosterone. It is also called salt-retaining hormone. It promotes reabsorption of sodium ions from kidney and excretion of potassium ions in urine. It also reabsorb Cl– ions from kidney. Thus aldosterone has a important contribution in homeostasis by controling osmatic pressure of ECF (Extra cellular fluid).
Remember that doctors administer saline drip to the patients who lose excessive water and salts due to diarrhoea, cholera, etc. Aldosterone also helps in maintaining acid-base equilibrium and blood pH (7.35) by promoting reabsorption of \[HC{{O}^{}}_{3}\] and regulating excretion of \[{{H}^{+}}\]by kidneys. It also promotes absorption of water and salt in intestine, mainly in colon. The Renin-angiotensin-aldosterone or RAA pathway controls more... 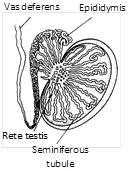
 Function
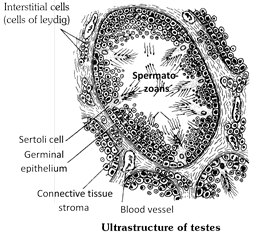
(1) It stimulates the male reproductive system to grow to full size and become functional.
(2) It stimulates the formation of sperms (spermatogenesis) in the seminiferous tubules.
(3) It stimulates the development of male accessory sex characters such as hair on the face (beard and moustaches), growth and distribution of hair on the body, thickening of skin, deepening of voice, enlargement of larynx, broadening of shoulders, Narrow lips enlarged and stronger bones and muscles. It also maintains these characters.
(4) It also determines the male sexual behaviour sex urge, aggressive behaviour.
(5) Under its effect protein anabolism increases. (This function is obvious in the heavier muscle and bone mass of most men as compared to women).
(6) Grythropoisis in bone marrow increases.
(7) In brief, testosterone determines libido or sex drive. It is also required, together with the follicle stimulating hormone (FSH) of pituitary, for initiation and completion of spermatogenesis. All androgens are also secreted in traces from adrenal glands in both boys and girls.
(8) Increased sebaceous gland secretion.
Development of testis : Under the effect of chorionic gonadotropic hormone, secreted by placenta during pregnancy, the testes of eight to nine months old fetus start secreting testosterone. The latter regulates differentiation and development of urinogenital system, accessory genital organs and external genitalia in the embryo. During childhood i.e. from birth to puberty (age of 11 to 13 years), testes remain quiescent, so that androgens are not secreted. At puberty, the gonadotropic hormones (FSH and ICSH) of pituitary reactivate the testes which, therefore, start producing sperms and resume secreting androgens. Upto the age of about 40 years, androgens are secreted in sufficient amounts. There after, their secretion starts gradually declining, but the capability of reproduction still continues for many years.
Castration : Surgical removal of testes is called castration or orchidectomy. Castration, or deficient secretion of testosterone (hypogonadism) before puberty (due to congenital defects or injury to testes) retards growth of genitalia, muscles and bones, as well more...
Function
(1) It stimulates the male reproductive system to grow to full size and become functional.
(2) It stimulates the formation of sperms (spermatogenesis) in the seminiferous tubules.
(3) It stimulates the development of male accessory sex characters such as hair on the face (beard and moustaches), growth and distribution of hair on the body, thickening of skin, deepening of voice, enlargement of larynx, broadening of shoulders, Narrow lips enlarged and stronger bones and muscles. It also maintains these characters.
(4) It also determines the male sexual behaviour sex urge, aggressive behaviour.
(5) Under its effect protein anabolism increases. (This function is obvious in the heavier muscle and bone mass of most men as compared to women).
(6) Grythropoisis in bone marrow increases.
(7) In brief, testosterone determines libido or sex drive. It is also required, together with the follicle stimulating hormone (FSH) of pituitary, for initiation and completion of spermatogenesis. All androgens are also secreted in traces from adrenal glands in both boys and girls.
(8) Increased sebaceous gland secretion.
Development of testis : Under the effect of chorionic gonadotropic hormone, secreted by placenta during pregnancy, the testes of eight to nine months old fetus start secreting testosterone. The latter regulates differentiation and development of urinogenital system, accessory genital organs and external genitalia in the embryo. During childhood i.e. from birth to puberty (age of 11 to 13 years), testes remain quiescent, so that androgens are not secreted. At puberty, the gonadotropic hormones (FSH and ICSH) of pituitary reactivate the testes which, therefore, start producing sperms and resume secreting androgens. Upto the age of about 40 years, androgens are secreted in sufficient amounts. There after, their secretion starts gradually declining, but the capability of reproduction still continues for many years.
Castration : Surgical removal of testes is called castration or orchidectomy. Castration, or deficient secretion of testosterone (hypogonadism) before puberty (due to congenital defects or injury to testes) retards growth of genitalia, muscles and bones, as well more... | S.No. | Neurohormones | Physiological effects |
| 1. | TRH (Thyroid Releasing Hormone - Releasing Factor) | Increased TSH secretion from adenohypophysis. |
| 2. | ACTH-RF (Adrenocorticotrophic Hormone-Releasing Factor) | Increased ACTH secretion from adenohypophysis. |
| 3. | STH-RF | |
| more...
Hormones described so far are called circulating hormones, because these circulate in whole body with blood. When stimulated by physical or chemical stimuli, all body cells, except red blood corpuscles (RBCs), secrete certain such compounds which transmit coded informations of metabolic adjustments between neighbouring cells and hence remain ECF instead of diffusing into the blood. These compounds are called local tissue hormones or autocoids. These are short-lived, because various enzymes present in ECF continue degrading these at a fast rate.
Local hormones are of two main categories-paracrine and autocrine. Paracrine hormones affect metabolism of cells located in the neighbourhood of those which secrete them. Autocrine hormones affect metabolism of the every cells which secrete them. Most local hormones are paracrine. These belong to the following categories :
(1) Eicosanoids : These are a category of lipids derived from a fatty acid, arachidonic acid, synthesized in the plasma membrane of cells, and released in ECF. These are of four categories, viz. Prostaglandins, prostacyclins, thromoboxanes and leukotrienes.
(i) Prostaglandins (PGs) : In 1935, Ulf von Euler discovered that human semen contains a very active compound presumably secreted by prostate gland and, hence, named as such. He found that after the semen is discharged in woman’s vagina, this compound contracts uterine muscles to facilitate the sperms to ascend into fallopian tubes and reach ova to fertilize these.
(ii) Prostacyclins : These are found in walls of blood vessels and induce vasodilation. These also facilitate flow of blood in vessels and prevent thrombosis by inhibiting aggregation of platelets.
(iii) Thromboxanes : These are secreted by blood platelets. These help in blood clotting by instigating aggregation of platelets at the place of injury. These also instigate vasoconstriction at places of injury to prevent excessive loss of blood.
(iv) Leukotrienes : These are secreted by eiosinophils of blood and mast cells of connective tissues. These serve as mediators in inflammatory and allergic reactions, induce bronchoconstriction (constriction of bronchioles), constrict arterioles and induce migration of neutrophils and eosinophils towards the places of inflammation. These can cause asthma, arthritis, colitis, etc.
(2) Neuroregulators : These are a category of proteins which function as paracrine hormones in nervous tissues. These can be classified in three categories as follows :
(i) Neurotransmitters : These are synthesized in nerve cells and are secreted by exocytosis by axon terminals of these cells. These serve to transmit nerve impulses from one neuron to other neighbouring neurons, or muscles, or glands across synapses. About 60 to these have so far been discovered, but the most common of these are acetylcholine, norepinephrine, dopamine, serotonin and histamine.
(ii) Neuromodulators : In nervous tissues, the neurons secrete such paracrine hormones which modulate (increase or decrease) the excitability of other neighbouring neurons. These hormones are called neuromodulators. The main positive neuromodulators which increase the excitability of other neurons are the amino acids glutamate and aspartate, and polypeptide named ‘P’ substance. Contrarily, the main negative modulators which decrease the excitability of neighbouring neurons are the amino acid glycine and more...
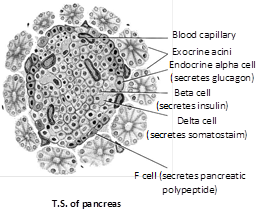
Location and origin : Pancreas (Gr. pankreas = sweet bread; Fr., pan = all + kreas = flesh) is a flattened and pinkish mixed gland (both exocrine and endocrine) situated in the concavity formed by duodenum just behind the stomach. It measures about 15 cm in length and 4 to 5 cm in breadth. It forms by fusion of two bilateral endodermal processes of embyronic intestine (duodenum of future adult).
Structure : About 99% part of the gland is exocrine and formed of hollow pancreatic acini or lobules embedded in a connective tissue stroma. In the stroma, there are numerous (approximately 1 to 2 million in human pancreas) small (0.1 to 0.2 mm in diameter) clusters of endocrine cells, called islets of Langerhans after the name of their discoverer, Paul Langerhans (1869).
 Cells Types in the Pancreatic Islets
Each pancreatic islet includes four types of hormone-secreting cells :
(1) Alpha or A cells constitute about 15% of pancreatic islet cells and secrete glucagon.
(2) Beta or B cells constitute about 80% of pancreatic islet cells and secrete insulin.
(3) Delta or D cells : It’s constitute about 5% of pancreatic islet cells and secrete somatostatin (identical to growth hormone-inhibiting hormone secreted by the hypothalamus).
(4) F cells : It’s constitute the remainder of pancreatic islet cells and secrete pancreatic polypeptide.
Hormones of pancreas and their role
The \[\beta \] and \[\alpha \] cells of islets of Langerhans respectively secrete insulin and glucagon hormones which are important regulation of carbohydrate, protein and fat metabolism in the body.
(1) Insulin : In 1889, Minkowski and Mehring discovered that pancreas is related with the disease of diabetes mellitus in humans. Normal concentration of glucose in blood is about 100 mg (0.1 gm) per 100 ml. It increases somewhat after a carbohydrate rich food. Then, the secretion of insulin increases. It increases the permeability of all cells for glucose several times, except that of brain cells and red blood corpuscles (RBCs). The brain cells and RBCs are already highly permeable to glucose. After taking more glucose from blood, the cells utilize it for energy-production. Consequently, the basal metabolic rate (BMR) and RNA and protein synthesis increases in cells.
In 1923, two Canadian scientists, Banting and Best succeeded in preparing a pure extract of insulin from the pancreatic islets of a new born calf with the help of Macleod, Banting and Macleod won the 1923 Nobel prize for this work. Later, Abel (1926) succeeded in preparing pure crystals of insulin. F. Sanger (1955) worked out the molecular structure of bovine insulin and won the 1958 Nobel Prize. He discovered that insulin is a small protein whose molecule consists of two polypeptide chains, \[\alpha \]and \[\beta ,\] joined by disulphide linkages and respectively formed of 21 and 30 amino acid residues. Insulin is the first protein to be crystallized in pure form, first protein whose molecular structure was worked out, more...
Cells Types in the Pancreatic Islets
Each pancreatic islet includes four types of hormone-secreting cells :
(1) Alpha or A cells constitute about 15% of pancreatic islet cells and secrete glucagon.
(2) Beta or B cells constitute about 80% of pancreatic islet cells and secrete insulin.
(3) Delta or D cells : It’s constitute about 5% of pancreatic islet cells and secrete somatostatin (identical to growth hormone-inhibiting hormone secreted by the hypothalamus).
(4) F cells : It’s constitute the remainder of pancreatic islet cells and secrete pancreatic polypeptide.
Hormones of pancreas and their role
The \[\beta \] and \[\alpha \] cells of islets of Langerhans respectively secrete insulin and glucagon hormones which are important regulation of carbohydrate, protein and fat metabolism in the body.
(1) Insulin : In 1889, Minkowski and Mehring discovered that pancreas is related with the disease of diabetes mellitus in humans. Normal concentration of glucose in blood is about 100 mg (0.1 gm) per 100 ml. It increases somewhat after a carbohydrate rich food. Then, the secretion of insulin increases. It increases the permeability of all cells for glucose several times, except that of brain cells and red blood corpuscles (RBCs). The brain cells and RBCs are already highly permeable to glucose. After taking more glucose from blood, the cells utilize it for energy-production. Consequently, the basal metabolic rate (BMR) and RNA and protein synthesis increases in cells.
In 1923, two Canadian scientists, Banting and Best succeeded in preparing a pure extract of insulin from the pancreatic islets of a new born calf with the help of Macleod, Banting and Macleod won the 1923 Nobel prize for this work. Later, Abel (1926) succeeded in preparing pure crystals of insulin. F. Sanger (1955) worked out the molecular structure of bovine insulin and won the 1958 Nobel Prize. He discovered that insulin is a small protein whose molecule consists of two polypeptide chains, \[\alpha \]and \[\beta ,\] joined by disulphide linkages and respectively formed of 21 and 30 amino acid residues. Insulin is the first protein to be crystallized in pure form, first protein whose molecular structure was worked out, more...
(1) Position and structure : These are four in number which are wholly or partially embedded in the dorsal surface of the thyroid gland two glands in each lobe of thyroid gland. Each is oval shaped, small sized \[(5\times 5\text{ }mm)\] and yellow coloured. Histologically, a parathyroid gland is formed of masses of polygonal cell arranged in cords. Endocrine cell are two types principal or chief and oxyphil cells. Parathyroid is endodermal in origin.
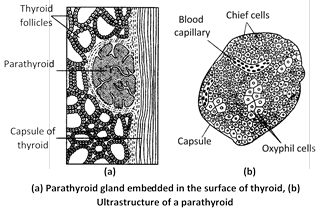 (2) Hormones of parathyroid : Active hormone secreted by parathyroids is parathormone (PTH), also called Collip's Hormone (Phillips collip, 1925). It was discovered and purified by Collip in 1925. Its crystals were first prepared by Craig and Ras mussen in 1960. Its molecular structure was worked out by potts and his associates in 1971. The latter is a protein of 84 amino acid monomer. It is a polypeptide hormone. Parathyroids are present in all vertebrates except fishes. Its secretion is stimulated by low level of calcium in blood than normal level through feedback control.
Functions of parathormone : Parathormone is essential for survival, because it significantly contributes to "homeostatis" by regulating the amount of calcium and phosphate ions in ECF. Our body requires an optimum calcium level (10.0 to 11.5 mg per 100mL.) in ECF (total 1000 to 1120 grams in a 70 kg man), because calcium is a key element in many physiological functions like proper permeability of cell membranes, muscular activities, nerve impulse conduction, heartbeat, blood coagulation, bone formation, fertilization of ova, etc. Calcium is most abundant of all minerals found in the body and about 99% of calcium and phosphorous are contained in the bones.
Maintenance of proper calcium level under 'homeostasis' is, in fact, a combined function of parathormone, thyrocalcitonin and vitamin D3 (cholecalciferol). Parathormone promotes absorption of calcium from food in the intestine and its reabsoption from nephrons in the kidneys. Simultaneously, it accelerates elimination of phosphates in urine (phosphaturic action). Thus, calcium level tends to rise in the ECF due to the effect of parathormone. This calcium is, then, utilized by bone-forming cells – osteoblast – in bone formation under the influence of vitamin D3. Bones are asymmetrical when first formed. Their unnecessary parts are, therefore, dissolved by bone-eating cells called osteoclasts. This process also proceeds under the influence of parathormone. It results in release of calcium and phosphate in blood.
Vitamin D3, is a steroid hormone which is first synthesized in an inactive form in skin cells from 7-dehydrocholesterol under the influence of ultraviolet (UV) rays of sunlight. Skin cells release it in blood. Liver cells take it from blood, change in into 25-hydroxycholecalciferol and release back into blood. Finally, the cells of proximal convoluted tubules of nephrons in the kidneys change 25-hydroxycholecalciferol into 1-25-dihydroxycholecalciferol under the influence of parathormone. This last compound is released in blood as active vitamin D3 named as cholecalciferol (calcitriol).
In addition to its role in bone-remodelling, D3 more...
(2) Hormones of parathyroid : Active hormone secreted by parathyroids is parathormone (PTH), also called Collip's Hormone (Phillips collip, 1925). It was discovered and purified by Collip in 1925. Its crystals were first prepared by Craig and Ras mussen in 1960. Its molecular structure was worked out by potts and his associates in 1971. The latter is a protein of 84 amino acid monomer. It is a polypeptide hormone. Parathyroids are present in all vertebrates except fishes. Its secretion is stimulated by low level of calcium in blood than normal level through feedback control.
Functions of parathormone : Parathormone is essential for survival, because it significantly contributes to "homeostatis" by regulating the amount of calcium and phosphate ions in ECF. Our body requires an optimum calcium level (10.0 to 11.5 mg per 100mL.) in ECF (total 1000 to 1120 grams in a 70 kg man), because calcium is a key element in many physiological functions like proper permeability of cell membranes, muscular activities, nerve impulse conduction, heartbeat, blood coagulation, bone formation, fertilization of ova, etc. Calcium is most abundant of all minerals found in the body and about 99% of calcium and phosphorous are contained in the bones.
Maintenance of proper calcium level under 'homeostasis' is, in fact, a combined function of parathormone, thyrocalcitonin and vitamin D3 (cholecalciferol). Parathormone promotes absorption of calcium from food in the intestine and its reabsoption from nephrons in the kidneys. Simultaneously, it accelerates elimination of phosphates in urine (phosphaturic action). Thus, calcium level tends to rise in the ECF due to the effect of parathormone. This calcium is, then, utilized by bone-forming cells – osteoblast – in bone formation under the influence of vitamin D3. Bones are asymmetrical when first formed. Their unnecessary parts are, therefore, dissolved by bone-eating cells called osteoclasts. This process also proceeds under the influence of parathormone. It results in release of calcium and phosphate in blood.
Vitamin D3, is a steroid hormone which is first synthesized in an inactive form in skin cells from 7-dehydrocholesterol under the influence of ultraviolet (UV) rays of sunlight. Skin cells release it in blood. Liver cells take it from blood, change in into 25-hydroxycholecalciferol and release back into blood. Finally, the cells of proximal convoluted tubules of nephrons in the kidneys change 25-hydroxycholecalciferol into 1-25-dihydroxycholecalciferol under the influence of parathormone. This last compound is released in blood as active vitamin D3 named as cholecalciferol (calcitriol).
In addition to its role in bone-remodelling, D3 more...
Origin, position and structure : This is a small, (0.1 to 0.29) whitish and somewhat flattened ectodermal gland situated at the tip of a small, fibrous stalk that arises from dorsal wall of diencephalon, i.e. the roof (epithalamus) of third ventricle of the brain. Due to its location, it is also called epiphysis cerebri. It is covered over by a thin capsule formed of the piamater of the brain. Septa from this membrane extend into the gland, dividing in into lobules having two types of branched cells, viz the large and modified nerve cells, called pinealocytes, and interstitial or neuroglial cells forming the supporting tissue. In the pineal gland starts degenerating after the age of about 7 years because of deposition of granules of calcium salts (brain sand) in it.
Function of pineal body : Hormone, though the function of the gland is still the subject of current research, it is known to secrete one hormone, melatonin. Melatonin concentration in the blood appears to flow a diurnal (day-night) cycle as it arises in the evening and through the night and drops to a low around noon. Melatonin lightens skin colour in certain animals and regulates working of gonads (testes and ovaries). Light falling on the retina of the eye decreases melatonin production, darkness stimulates melatonin synthesis. Girls blind from birth attain puberty earlier than normal, apparently because there is no inhibitory effect of melatonin on ovarian function.
Serotonin, a neurotransmitter found in other locations in the brain, is also found in the pineal gland. Research evidence is accumulating to support the idea that the pineal gland may be involved in regulating cyclic phenomena in the body. Melatonin also is a potent antioxidant. Melatonin causes atrophy of gonads in several animals.
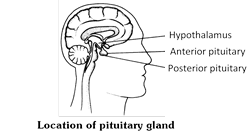
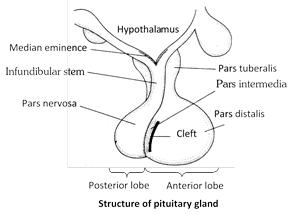
Pituitary is known as hypophysis cerebri, its name pituitary was given by Vesalius. Muller’s gland of amphioxus and subneural gland of hardmania is homologous to pituitary of vertebrates. Weight of pituitary is 0.5 gm. Removal of pituitary is knows as hypophysectomy.
Position and origin : Pituitary gland is the smallest (about 1 to 1½ cm in diameter) endocrine gland of the body. It is pea-shaped, ovoid, radish brown gland situated at the base of the brain in a cavity, hypophyseal fossa of the sella turcica of sphenoid bone. It is connected by a short stalk called Infundibulum, to the ventral wall (Hypothalamus) of diencephalon. That is why it is also called hypophysis cerebri. It weight about 0.5 to 1 gm. It control most of the endocrine glands. Hence, it is also called leader of endocrine orchestra or master gland. Pituitary gland is closely related with hypothalamus, hence, it is also called hypothalamo-hypophyseal gland, pituitary is ectodermal in origin.
Parts and component
Adenohypophysis
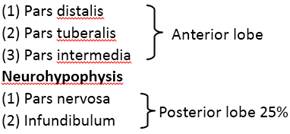
 Structure of pituitary gland : Pituitary gland is comprised of two main lobes – Adenohypophysis and Neurohypophysis. Adenohypophysis is arises as hypophysial or Rathke's pouch from dorsal wall of embyronic stomodeum. It is the anterior lobe of pituitary. The neurohypophysis (Pars nervosa or Posterior lobe) form as an outgrowth from the infundibulum of the floor of hypothalamus.
Structure of pituitary gland : Pituitary gland is comprised of two main lobes – Adenohypophysis and Neurohypophysis. Adenohypophysis is arises as hypophysial or Rathke's pouch from dorsal wall of embyronic stomodeum. It is the anterior lobe of pituitary. The neurohypophysis (Pars nervosa or Posterior lobe) form as an outgrowth from the infundibulum of the floor of hypothalamus.
 In pituitary following types of cells are found :
(1) Chromophobes cells : Found in adenohypophysis of pituitary. These are not stained by acid and base dye. Pigment granules are absent. These are colourless may change into chromophils.
(2) Chromophil cells : Found in adenohypophysis of pituitary. These are stained by acid and base dye. Pigment granules are filled in these cells. These may be two types :
(i) Acidophils : It is also known as a-cells synthesize and secretes growth hormone and prolactin.
(ii) Basophils : It is also known as cyanophils or b-cells synthesize and secretes TSH, ACTH, FSH, LH and MSH hormones.
(3) Pituicyte cells : These cells found in neurohypophysis of pituitary. These are supporting neuroglia cells and gives support to herring bodies.
(4) Herring bodies : Herring bodies Are dilated terminal portion of Neurosecretory axon constituting hypothalamohypophyseal tract. They are hormone precursors for oxytocin and vasopressin.
In pituitary following types of cells are found :
(1) Chromophobes cells : Found in adenohypophysis of pituitary. These are not stained by acid and base dye. Pigment granules are absent. These are colourless may change into chromophils.
(2) Chromophil cells : Found in adenohypophysis of pituitary. These are stained by acid and base dye. Pigment granules are filled in these cells. These may be two types :
(i) Acidophils : It is also known as a-cells synthesize and secretes growth hormone and prolactin.
(ii) Basophils : It is also known as cyanophils or b-cells synthesize and secretes TSH, ACTH, FSH, LH and MSH hormones.
(3) Pituicyte cells : These cells found in neurohypophysis of pituitary. These are supporting neuroglia cells and gives support to herring bodies.
(4) Herring bodies : Herring bodies Are dilated terminal portion of Neurosecretory axon constituting hypothalamohypophyseal tract. They are hormone precursors for oxytocin and vasopressin.
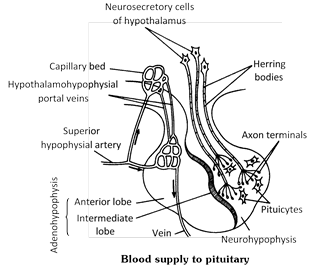 Blood supply to pituitary or Hypophyseal portal system : A pair of posterior hypophysial arteries and a pair of anterior hypophysial arteries provide blood to the pituitary gland. Posterior arteries supply blood to the pars nervosa, and anterior arteries supply blood to the hypothalamus and pars distalis. Adenohypophysis has dual blood supply by means of a "circle of willis". The anterior hypophysial artery which bring blood into this circle big ureates in to two branches outside the lobe. One more...
Blood supply to pituitary or Hypophyseal portal system : A pair of posterior hypophysial arteries and a pair of anterior hypophysial arteries provide blood to the pituitary gland. Posterior arteries supply blood to the pars nervosa, and anterior arteries supply blood to the hypothalamus and pars distalis. Adenohypophysis has dual blood supply by means of a "circle of willis". The anterior hypophysial artery which bring blood into this circle big ureates in to two branches outside the lobe. One more... Current Affairs CategoriesArchive
Trending Current Affairs
You need to login to perform this action. |