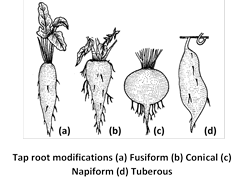
 (iv) Tuberous : The storage root having no definite shape is called tuberous, .e.g., Mirabilis jalapa (4 O’clock plant),
(2) Branched roots
(i) Nodular roots (Tuberculated roots) : The primary tap roots and its branches of leguminous plants, i.e., plants belonging to sub-family papilionatae of the family leguminosae (e.g., Pea, Gram, Ground nut, Beans etc.), bear nodule like swellings, called root nodules.
They are red in colour due to the presence of leg-haemoglobin. The nodules are inhabited by nitrogen fixing bacteria called Rhizobium leguminosarum. It converts atmospheric nitrogen into nitrates and supply them to the plant. In turn Rhizobium gets nutrients and shelter from the plant.
(ii) Pneumatophores or Respiratory roots : The roots of some plants growing in saline marshes (mangrove plants) suffer from the lack of oxygen. This is due to the water logged condition of the soil. To cope with this situation some root branches grow vertically upwards.
(iv) Tuberous : The storage root having no definite shape is called tuberous, .e.g., Mirabilis jalapa (4 O’clock plant),
(2) Branched roots
(i) Nodular roots (Tuberculated roots) : The primary tap roots and its branches of leguminous plants, i.e., plants belonging to sub-family papilionatae of the family leguminosae (e.g., Pea, Gram, Ground nut, Beans etc.), bear nodule like swellings, called root nodules.
They are red in colour due to the presence of leg-haemoglobin. The nodules are inhabited by nitrogen fixing bacteria called Rhizobium leguminosarum. It converts atmospheric nitrogen into nitrates and supply them to the plant. In turn Rhizobium gets nutrients and shelter from the plant.
(ii) Pneumatophores or Respiratory roots : The roots of some plants growing in saline marshes (mangrove plants) suffer from the lack of oxygen. This is due to the water logged condition of the soil. To cope with this situation some root branches grow vertically upwards.
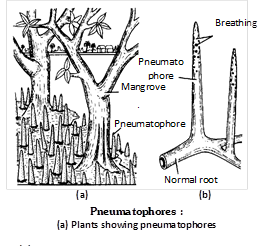 They become aerial and negatively geotropic. These roots bear many minute pores called pneumathodes (lenticels) towards their upper ends. Gaseous exchange takes place through pneumathodes. Such aerial, porous, roots which help in gaseous exchange are called breathing roots. e.g., Sonneratia, Heritiera, Rhizophora, Avicennia and Ceriops etc. and are found in sundarbans of West Bengal.
For physiological or Vital functions
(1) Storage roots : The roots where adventitious roots become swollen to store food. They are of following types :
Tuberous roots : These adventitious roots are swollen without any definite shape e.g., Ipomoea batata or (Sweet potato).
Fasciculated roots : These are tuberous roots arising in cluster from the base of the stem. e.g., Dahlia, Ruellia (Menow weed), Asparagus etc.
They become aerial and negatively geotropic. These roots bear many minute pores called pneumathodes (lenticels) towards their upper ends. Gaseous exchange takes place through pneumathodes. Such aerial, porous, roots which help in gaseous exchange are called breathing roots. e.g., Sonneratia, Heritiera, Rhizophora, Avicennia and Ceriops etc. and are found in sundarbans of West Bengal.
For physiological or Vital functions
(1) Storage roots : The roots where adventitious roots become swollen to store food. They are of following types :
Tuberous roots : These adventitious roots are swollen without any definite shape e.g., Ipomoea batata or (Sweet potato).
Fasciculated roots : These are tuberous roots arising in cluster from the base of the stem. e.g., Dahlia, Ruellia (Menow weed), Asparagus etc.
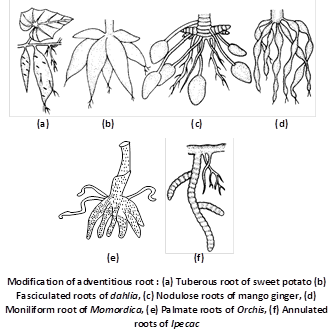 Nodulose roots : These roots become swollen at their tips due to accumulation of food e.g., Maranta sp. (Arrowroot), Curcuma amanda (Mango – ginger).
Moniliform or Beaded roots : These adventitious roots are swollen at frequent intervals. more...
Nodulose roots : These roots become swollen at their tips due to accumulation of food e.g., Maranta sp. (Arrowroot), Curcuma amanda (Mango – ginger).
Moniliform or Beaded roots : These adventitious roots are swollen at frequent intervals. more... | Roots | Stems | Leaves | |
| (i) Functions | (i) Absorb water and minerals. (ii) Anchor plant. (iii) Store materials. | (i) Transport water and nutrients. (ii) Support leaves. (iii) Help to store materials. | Carry on photosynthesis. |
| (ii) Tissues | |||
| (a) Epidermis | Root hairs absorb water and minerals. | Protect inner tissues. | Stomata carry on gas exchange. |
| (b) Cortex |
Store more...
The word “Meristem” originated from “Meristos” (Greek = continuous division) and the term meristem was introduced by Nageli (1858). A group of cells which are much active and capable of showing continuous divisions and redivisions, is called as meristematic tissue. The various characteristic features of the meristems are discussed below :
(1) They contain immature and young cells and are capable of repeated divisions.
(2) Intercellular spaces are not present in meristematic tissue.
(3) They contain a homogeneous thin cellulosic wall.
(4) They contain large nuclei associated with abundant cytoplasm.
(5) They are metabolically very active but they do not store food material and further no plastids in them.
(6) Vacuoles are small or absent.
(7) Meristematic cells are isodiametric in shape.
(8) Undifferentiated tissue in which cells divides continuously
Permanent tissues are made up of mature cells which have lost the capacity to divide and have attained a permanent shape, size and function due to division and differentiation in meristematic tissues. The cells of these tissues are either living or dead, thin-walled or thick-walled. Permanent tissues are of following types :
Simple permanent tissues
Simple tissues are a group of cells which are all alike in origin, form and function. They are further grouped under three categories :
(1) Parenchyma : Parenchyma is most simple and unspecialized tissue which is concerned mainly with the vegetative activities of the plant.
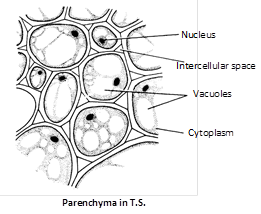 The main characteristics of parenchyma cells are :
(i) The cells are living, thin walled, soft, possess a distinct nucleus, having well developed intercellular spaces, vacuolated cytoplasm and cellulosic cell wall.
(ii) The shape may be oval, spherical, cylindrical, rectangular and stellate (star shaped) in leaf petioles of banana and canna and some hydrophytes.
(iii) This tissue is generally present in roots, stems, leaves, flowers, fruits and seeds.
(iv) If they enclose large air spaces they are called as aerenchyma; if they develop chlorophyll, they are called as chlorenchyma and if they are elongated cells with tapering ends, they are called as prosenchyma.
Functions : They perform the following functions :
(i) Storage of food materials. e.g., Carrot, Beetroot etc.
(ii) Chlorenchyma helps in photosynthesis. Aerenchyma helps in floating of the aquatic plants (Hydrophytes) and also helps in gaseous exchange during respiration and photosynthesis. e.g., Hydrilla.
(iii) In turgid state they give rigidity to the plant organs.
(iv) In emergency they behave like meristematic cells and help in healing of the various plant injuries.
(v) Sometimes they store secretory substances (ergastic substance) such as tannins, resins and gums and they are called as idioblasts.
(2) Collenchyma : The term collenchyma was coined by Schleiden (1839). It is the tissue of primary body. The main characteristics of collenchyma are given below :
(i) The cells of this tissue contain protoplasm and are living without intercellular spaces. The cell walls are thickened at the corners and are made up of cellulose, hemicellulose and pectin.
(ii) They are compactly arranged cells, oval, spherical or polygonal in outline. The tissue is elastic, extensible and have capacity to expand.
(iii) Collenchyma occurs chiefly in the hypodermis of dicotyledonous stems (herbaceous, climbers or plants e.g. Cucurbita, Helianthus) and leaves. They are usually absent in monocots and in roots.
The main characteristics of parenchyma cells are :
(i) The cells are living, thin walled, soft, possess a distinct nucleus, having well developed intercellular spaces, vacuolated cytoplasm and cellulosic cell wall.
(ii) The shape may be oval, spherical, cylindrical, rectangular and stellate (star shaped) in leaf petioles of banana and canna and some hydrophytes.
(iii) This tissue is generally present in roots, stems, leaves, flowers, fruits and seeds.
(iv) If they enclose large air spaces they are called as aerenchyma; if they develop chlorophyll, they are called as chlorenchyma and if they are elongated cells with tapering ends, they are called as prosenchyma.
Functions : They perform the following functions :
(i) Storage of food materials. e.g., Carrot, Beetroot etc.
(ii) Chlorenchyma helps in photosynthesis. Aerenchyma helps in floating of the aquatic plants (Hydrophytes) and also helps in gaseous exchange during respiration and photosynthesis. e.g., Hydrilla.
(iii) In turgid state they give rigidity to the plant organs.
(iv) In emergency they behave like meristematic cells and help in healing of the various plant injuries.
(v) Sometimes they store secretory substances (ergastic substance) such as tannins, resins and gums and they are called as idioblasts.
(2) Collenchyma : The term collenchyma was coined by Schleiden (1839). It is the tissue of primary body. The main characteristics of collenchyma are given below :
(i) The cells of this tissue contain protoplasm and are living without intercellular spaces. The cell walls are thickened at the corners and are made up of cellulose, hemicellulose and pectin.
(ii) They are compactly arranged cells, oval, spherical or polygonal in outline. The tissue is elastic, extensible and have capacity to expand.
(iii) Collenchyma occurs chiefly in the hypodermis of dicotyledonous stems (herbaceous, climbers or plants e.g. Cucurbita, Helianthus) and leaves. They are usually absent in monocots and in roots.
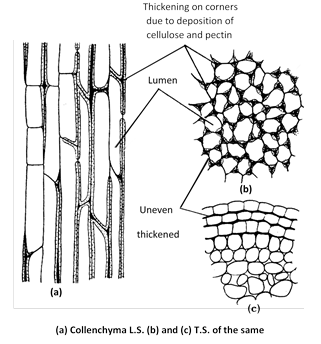 Types of collenchyma : Majumdar (1941) divided collenchyma into three types on the basis of thickening :
(i) Angular collenchyma : When the thickening of the cells is confined to the corners of the cells. e.g., Tagetes, Tomato, Datura, Potato, etc.
(ii) Plate or Lamellar collenchyma : When the thickenings are present in the tangential walls. e.g. hypodermis of sunflower stem.
(iii) Lacunar or Tubular collenchyma : If the thickened cell wall is associated with intercellular spaces of more...
Types of collenchyma : Majumdar (1941) divided collenchyma into three types on the basis of thickening :
(i) Angular collenchyma : When the thickening of the cells is confined to the corners of the cells. e.g., Tagetes, Tomato, Datura, Potato, etc.
(ii) Plate or Lamellar collenchyma : When the thickenings are present in the tangential walls. e.g. hypodermis of sunflower stem.
(iii) Lacunar or Tubular collenchyma : If the thickened cell wall is associated with intercellular spaces of more...
The increase in thickness or girth due to the activity of the cambium and the cork cambium is known as secondary growth.
(1) Secondary growth in stem : On the basis of the activities of cambium and cork-cambium, secondary growth in stem can be discussed under the following heads :
Activity of cambium : The vascular cambium in between xylem and phloem is called intrafascicular or fascicular cambium which is primary in origin. At the time of secondary growth the parenchymatous cells of medullary rays between the vascular bundles become meristematic and form strip of cambium called as interfascicular cambium which is secondary in origin. Both inter and intrafascicular cambium joins together and form cambium ring which is partly primary and partly secondary in origin. By anticlinal divisions the circumference of the cambium increase. By periclinal division cambium produces the secondary xylem and phloem tissues on innerside and outerside. The amount of sec. xylem produced is 8-10 times greater than sec. phloem. The cambium has two types of cells :
The fusiform initials : Which are elongated and form fibres, sieve cells, sieve tubes, tracheids.
Ray initials : Which produce parenchyma cells of the rays in wood and phloem. Certain cells of cambium form some narrow bands of living parenchyma cells passing through secondary xylem and secondary phloem and are called secondary medullary rays. These provide radial conduction of food from the phloem, and water and mineral salts from the xylem.
Annual rings : Activity of cambium is not uniform in those plants which grow in the regions where favourable climatic conditions (spring or rainy season) alternate regularly with unfavourable climatic conditions (cold water or dry hot summer). In temperate climates, cambium becomes more active in spring and forms greater number of vessels with wider cavities; while in winter it becomes less active and forms narrower and smaller vessels. The wood formed in the spring is known as spring wood and that formed in the dry summer or cold winter autumn wood or late wood. Both autumn and spring wood constitute a growth or annual ring. In one year only one growth ring is formed. Spring wood is light in colour while autumn wood is dark in colour.
Activity of cork cambium : Cork cambium or phellogen develops from outer layer of cortex. It produces secondary cortex or phelloderm on innerside and cork or phellem on outerside. The cells of phellem are dead, suberized and impervious to water. Cells of phelloderm are thin walled, living and store food. Phellem, phellogen and phelloderm are collectively called as periderm. Periderm is secondary protective tissue. Due to pressure of secondary xylem, epidermis ruptures and cortex is largely lost after two or three years of secondary growth.
Bark : All dead tissues lying outside the active cork-cambium are collectively known as bark. This includes ruptured epidermis, hypodermis and cork. When cork-cambium appears in the form of a complete ring, it is known as ring bark, e.g., Betula (Bhojpatra). If the cork cambium occurs as more...
These tissue perform special function in plants, e.g., secretion of resins gum, oil and latex.
These tissues are of two types :
(1) Laticiferous tissues : They are made up of thin walled, elongated, branched and multinucleate (coenocytic) structures that contain colourless, milky or yellow coloured juice called latex. These occur irregularly distributed in the mass of parenchymatous cells. Latex is contained inside the laticiferous tissue which is of two types :
(i) Latex cells : A laticiferous cell is a highly branched cell with long slender processes ramifying in all directions in the ground tissue of the organ. They do not fuse and do not form network. Plants having such tissues are called simple or non-articulated laticifers. e.g., Calotropis (Asclepiadaceae) Nerium, Vinca (Apocyanaceae), Euphorbia (Euphorbiaceae), Ficus (Moraceae).
(ii) Latex vessels : They are formed due to fusion of cells and form network like structure in all directions. At maturity, they form a highly ramifying system of channels full of latex inside the organ. Plants having such tissues are called compound or articulated laticifers. e.g., Argemone, Papaver (Papaveraceae), Sonchus (Compositae), Hevea, Manihot (Euphorbiaceae).
(2) Glandular tissue : This is a highly specialized tissue consisting of glands, discharging diverse functions, including secretory and excretory. Glands may be external or internal.
(i) External glands : They generally occur on the epidermis of stem and leaves as glandular hair in Plumbago and Boerhaavia, stinging hair secrete poisonous substance in Urtica dioica, nectar secreting glands in flowers or leaves. e.g., Rutaceae and Euphorbiaceae. Digestive enzyme secreting glands in insectivorous plants e.g., Drosera (Sundew), Nepenthes (Pitcher plant).
(ii) Internal glands : These are present internally and are of several types. e.g., oil glands in Citrus and Eucalyptus, resinous ducts in Pinus, mucilage canals in Cycas. Water secreting glands (hydathodes) in Colocasia (present at the tip of leaves), Tropaeoleum (along margin), etc. The glands which secrete essential oil are called osmophores (osmotrophs).
Several tissues may collectively perform the same function. A collection of tissues performing the same general function is known as a “Tissue System''. According to Sachs (1975) there are three major tissue systems in plants as follows :
(1) Epidermal tissue system : The tissues of this system originate from the outermost layer of apical meristem. It forms the outermost covering of various plant organs which remains in direct contact with the environment.
Epidermis : Epidermis is composed of single layer of cells. These cells vary in their shape and size and form a continuous layer interrupted by stomata. In some cases epidermis may be multilayered e.g. Ficus, Nerium, Peperomia, Begonia etc.
The epidermal cells are living, parenchymatous, and compactly arranged without intercellular spaces.
Certain epidermal cells of some plants or plant parts are differentiated into variety of cell types :
(i) In aerial roots, the multiple epidermal cells are modified to velamen, which absorbs water from the atmosphere (e.g., Orchids).
(ii) Some of the cells in the leaves of grasses are comparatively very large, called bulliform or motor cells. It is hygroscopic in nature. e.g., Ammophila. They are thin-walled and contain big central vacuoles filled with water. They play an important role in the folding and unfolding of leaves.
(iii) Some members of Gramineae and Cyperaceae possess two types of epidermal cells : the long cells and the short cells. The short cells may be cork cells or silica cells.
Cuticle and Wax : In aerial parts, epidermis is covered by cuticle. The epidermal cells secrete a waxy substance called cutin, which forms a layer of variable thickness (the cuticle) within and on the outer surface of its all walls. It helps in reducing the loss of water by evaporation. Usually the cuticle is covered with wax which may be deposited in the form of granules, rods, crusts or viscous semiliquid masses. Other substances deposited on the cuticle surface may be oil, resin, silicon and salts (cystoliths are crystals of calcium carbonate, e.g., Ficus. Druse and Raphides, e.g., Pistia are crystals of calcium oxalate). Thick cuticle are found in leaves of dry habitats plants.
Stomata : Stomata are minute apertures in the epidermis. Each aperture is bounded by two kidney shaped cells, called guard cells. Stomata are absent in roots. In xerophytes the stomata are sunken in grooves due to which rate of transpiration is greatly reduced (e.g. Nerium). Usually there is a large air cavity below each aperture, it is called substomatal cavity. In some species the guard cells are surrounded by subsidiary cells or accessory cells which differ morphologically as well as ontogenitally from the other epidermal cells. In monocots subsidiary cells and guard cells originated from same cell. e.g., Doob, Maize guard cells are dumb bell shape. Stomata are scattered in dicots leaves but they are arranged in rows in monocots.
Trichomes : These are epidermal outgrowths present temporarily or permanently on almost all plant parts. They may be unicellular or multicellular and vary in size more...
It can be defined as modified dwarf shoot which is meant for sexual reproduction. It is characteristic feature of angiosperm.
Parts of a typical flower : A typical flower of an angiosperm consists of four types of floral parts namely calyx, corolla, androecium and gynoecium.
General description of a flower
The flowers are termed pedicellate if they possess stalks and sessile if they lack them. The flower may be described as complete if it bears all the floral parts and incomplete, when one or more floral parts are absent. Flowers are called bisexual if they bear both androecium and gynoecium. The unisexual flowers have either androecium or gynoecium. The unisexual flowers may be male flowers or female flowers. The male flower are also called staminate flowers as they have stamens only.
The female flowers have only the carpels and hence called pistillate flowers. Flowers with sterile sex organs are described as neutral flowers. According to the distribution of male, female and bisexual flowers, various patterns are recognized.
Monoecious : Presence of male and female flowers on the same plant, e.g., Acalypha, Cocos and Ricinus.
Dioecious : Presence of male and female flowers on different plants, namely, male plants and female plants. e.g., Cycas, Carica papaya and Vallisneria.
Polygamous : Presence of unisexual and bisexual flowers on the same plant, e.g., Mangifera and Polygonum.
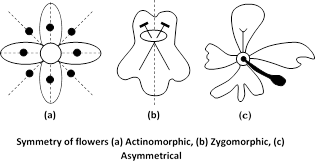
Symmetry of flower
The number, shape, size and arrangement of floral organs in a flower determines its symmetry. On the basis of symmetry flowers can be of the following types :
Actinomorphic (Regular = Symmetrical) : Actinomorphic flowers can be divided (passing through center) by any vertical plane into two equal and similar halves. e.g., Mustard, Brinjal, Catharanthus roseus.
Zygomorphic (Monosymmetrical) : Zygomorphic flowers can be divided into two equal halves by only one vertical division e.g., Pea, Larkspur, Ocimum.
Asymmetrical (Irregular) : Asymmetrical flowers can not be divided into two equal halves by any vertical division. e.g., Canna, Orchids.
 Arrangement of floral organs
On the basis of arrangement of floral organs, three types of flowers are recognized. They are :
Acyclic : Here the thalamus is conical or convex and the floral parts are spirally arranged, e.g., Water lily and Magnolia.
Cyclic : Here the floral organs are arranged in regular whorls at the nodes of the thalamus, e.g., Hibiscus and Datura.
Hemicyclic (Spirocyclic) : Here some floral parts (sepals and petals) are arranged in regular whorls and the remaining parts (stamens and carpels) are arranged spirally. e.g., Annona and Polyalthia.
Number of floral parts in whorl is called the merosity. There are two kinds of flowers based on the merosity of the flower. They are isomerous flowers and anisomerous flowers.
If the number of sepals, petals, stamens and carpels of flower is equal, such flowers are called isomerous flowers.
Dimerous : Two floral parts in each whorl. e.g., Poppy flower.
Trimerous : Three floral parts in each whorl. e.g., Monocot flowers (Liliaceae).
Tetramerous : Four more...
Arrangement of floral organs
On the basis of arrangement of floral organs, three types of flowers are recognized. They are :
Acyclic : Here the thalamus is conical or convex and the floral parts are spirally arranged, e.g., Water lily and Magnolia.
Cyclic : Here the floral organs are arranged in regular whorls at the nodes of the thalamus, e.g., Hibiscus and Datura.
Hemicyclic (Spirocyclic) : Here some floral parts (sepals and petals) are arranged in regular whorls and the remaining parts (stamens and carpels) are arranged spirally. e.g., Annona and Polyalthia.
Number of floral parts in whorl is called the merosity. There are two kinds of flowers based on the merosity of the flower. They are isomerous flowers and anisomerous flowers.
If the number of sepals, petals, stamens and carpels of flower is equal, such flowers are called isomerous flowers.
Dimerous : Two floral parts in each whorl. e.g., Poppy flower.
Trimerous : Three floral parts in each whorl. e.g., Monocot flowers (Liliaceae).
Tetramerous : Four more...
The flowers are arranged in some definite manner on the plant in each species of the flowering plants. The mode of arrangement of flowers on a specialised branch on top of the plant which bears flowers is called inflorescence. The stalk of the inflorescence is called peduncle.
Depending upon the arrangement of flowers, inflorescence is classified as follows :
 Current Affairs CategoriesArchive
Trending Current Affairs
You need to login to perform this action. |